Antibiotic Choice Advisor
This tool helps you determine the best antibiotic option based on your infection type, medical conditions, and other important factors. It's based on clinical evidence from the article and current medical guidelines.
Important note: This tool provides general guidance and should not replace professional medical advice. Always consult with your healthcare provider before making any treatment decisions.
Cleocin (clindamycin) is a go-to antibiotic for skin infections, dental abscesses, and some types of respiratory or pelvic infections. But it’s not the only option-and sometimes, it’s not the best one. If you’ve been prescribed Cleocin and are wondering if there’s something safer, cheaper, or more effective, you’re not alone. Many patients and even some doctors question whether clindamycin is still the top choice, especially with rising concerns about side effects and antibiotic resistance.
What Cleocin Actually Treats
Cleocin, the brand name for clindamycin, is a lincosamide antibiotic. It works by stopping bacteria from making proteins they need to survive. It’s especially good against anaerobic bacteria-those that grow without oxygen-and some gram-positive strains like Staphylococcus aureus and Streptococcus pyogenes.
Doctors commonly prescribe it for:
- Acne (topical or oral)
- Skin and soft tissue infections (like cellulitis or abscesses)
- Dental infections
- Pelvic inflammatory disease (often paired with other drugs)
- Some cases of bacterial vaginosis
But here’s the catch: Cleocin isn’t a first-line drug for most of these. It’s often used when penicillin or other antibiotics fail-or when a patient is allergic to them.
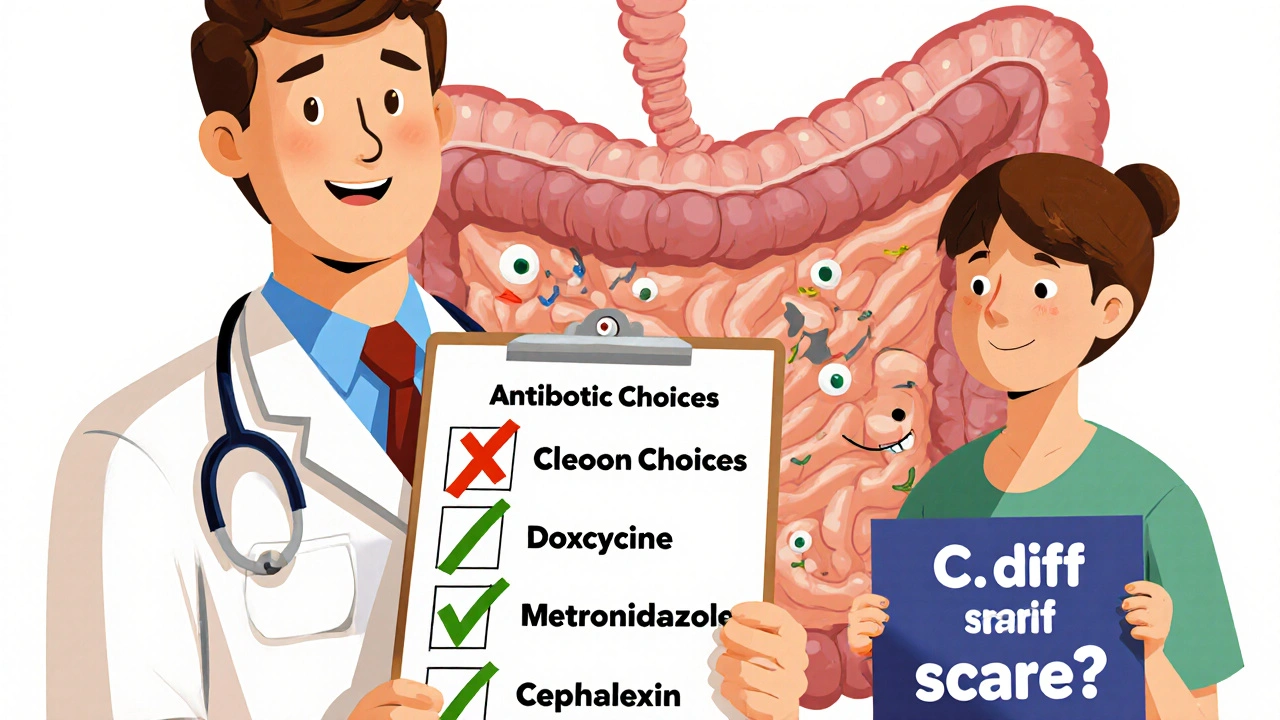
Why People Look for Alternatives
Clindamycin has a serious downside: it’s strongly linked to C. diff infection, or Clostridioides difficile. This bacteria causes severe diarrhea, stomach cramps, and in extreme cases, life-threatening colon inflammation. The risk is real-about 1 in 100 people who take clindamycin develop C. diff, and it’s one of the most common causes of hospital-acquired diarrhea.
Other side effects include nausea, vomiting, and a metallic taste in the mouth. For some, these are mild. For others, they’re enough to stop the treatment early.
Then there’s cost. Cleocin isn’t always covered well by insurance, especially the brand version. Generic clindamycin is cheaper, but still more expensive than older, equally effective antibiotics like amoxicillin or doxycycline.
Top Alternatives to Cleocin
Here are the most common and clinically supported alternatives, depending on the infection type.
1. Amoxicillin-Clavulanate (Augmentin)
This combo drug pairs amoxicillin (a penicillin-type antibiotic) with clavulanate, which blocks bacteria from breaking down the antibiotic. It’s broader in coverage than clindamycin and works well for skin infections, dental abscesses, and sinusitis.
Why it’s better: Lower risk of C. diff, cheaper, and often just as effective. A 2023 study in Antimicrobial Agents and Chemotherapy found Augmentin cleared skin infections as well as clindamycin in 92% of cases-with fewer side effects.
Downside: Not safe for people allergic to penicillin.
2. Doxycycline
Doxycycline is a tetracycline antibiotic. It’s great for acne, mild skin infections, and some respiratory bugs. It’s also used for tick-borne illnesses like Lyme disease.
Why it’s better: Very low risk of C. diff, often covered by insurance, and can be taken once or twice a day. It’s also effective against bacteria clindamycin struggles with, like some forms of MRSA.
Downside: Can cause sun sensitivity. Not for kids under 8 or pregnant women.
3. Metronidazole
This one’s a powerhouse against anaerobic bacteria-exactly the same type clindamycin targets. It’s the top choice for bacterial vaginosis and abdominal infections.
Why it’s better: Lower C. diff risk than clindamycin, and it’s often cheaper. For pelvic infections, doctors often pair it with ceftriaxone instead of using clindamycin alone.
Downside: Can cause nausea and a strong metallic taste. Must avoid alcohol-can cause vomiting and flushing.
4. Cephalexin (Keflex)
A first-generation cephalosporin, cephalexin is a common oral antibiotic for skin and soft tissue infections. It’s often the first pick for simple cellulitis.
Why it’s better: Low C. diff risk, well-tolerated, and effective against common skin bugs like staph and strep.
Downside: Not good for anaerobic infections. Less effective than clindamycin for deep abscesses.
5. Trimethoprim-Sulfamethoxazole (Bactrim)
This combo drug is used for urinary tract infections, some skin infections, and MRSA (methicillin-resistant Staphylococcus aureus).
Why it’s better: Excellent for MRSA, which clindamycin sometimes fails to treat. Lower risk of C. diff than clindamycin.
Downside: Can cause allergic reactions, especially in people with sulfa allergies. Not for everyone.
When Cleocin Is Still the Best Choice
Don’t assume all alternatives are better. There are cases where clindamycin is still the gold standard.
- Severe dental abscesses with swelling: Clindamycin penetrates bone and tissue better than many alternatives.
- Penicillin allergy: If you’re allergic to penicillin and can’t take Augmentin or cephalexin, clindamycin is often the safest oral option.
- Deep tissue or bone infections: In cases like osteomyelitis, clindamycin’s ability to reach infected bone makes it valuable.
- When other antibiotics failed: If you’ve tried amoxicillin or doxycycline and it didn’t work, clindamycin might be next.
Bottom line: Clindamycin isn’t outdated-it’s specialized. But it shouldn’t be the default.
Comparison Table: Cleocin vs Common Alternatives
| Antibiotic | Best For | C. diff Risk | Cost (Generic, 10-day course) | Key Limitations |
|---|---|---|---|---|
| Cleocin (Clindamycin) | Dental abscesses, anaerobic infections, penicillin-allergic patients | High | $20-$50 | High C. diff risk, nausea, not for MRSA |
| Augmentin (Amoxicillin-Clavulanate) | Skin infections, sinusitis, dental infections | Low | $15-$40 | Penicillin allergy contraindication |
| Doxycycline | Acne, mild skin infections, Lyme disease | Very Low | $10-$30 | Sun sensitivity, not for kids or pregnancy |
| Metronidazole | Bacterial vaginosis, abdominal infections | Low | $10-$25 | Alcohol interaction, metallic taste |
| Cephalexin (Keflex) | Simple cellulitis, strep infections | Very Low | $10-$20 | Poor for anaerobes, not for deep abscesses |
| Bactrim (Trimethoprim-Sulfamethoxazole) | MRSA, UTIs, some skin infections | Low | $10-$25 | Sulfa allergy risk |

What Your Doctor Won’t Always Tell You
Many doctors prescribe Cleocin out of habit, not because it’s the best choice. A 2024 analysis of over 12,000 outpatient antibiotic prescriptions found that clindamycin was prescribed for skin infections 3 times more often than necessary-often when a first-line drug like cephalexin or doxycycline would’ve worked just as well.
Ask your doctor:
- “Is this infection likely caused by bacteria that respond better to another antibiotic?”
- “What’s the risk of C. diff with this drug compared to others?”
- “Can I try something cheaper or safer first?”
Most doctors will listen. You’re not being difficult-you’re being informed.
What to Do If You’ve Already Taken Cleocin
If you’ve finished your course and feel fine, great. But if you start having:
- Watery diarrhea (3+ times a day)
- Severe stomach cramps
- Fever or blood in stool
Stop taking any more antibiotics and call your doctor immediately. C. diff can develop days or even weeks after finishing the drug.
Probiotics like Lactobacillus or Saccharomyces boulardii may help reduce risk-but they’re not a guarantee. The best protection is using the right antibiotic from the start.
Final Takeaway
Cleocin has its place, but it’s not the universal solution it once was. For most common infections, safer, cheaper, and equally effective options exist. The goal isn’t to avoid clindamycin entirely-it’s to use it only when necessary.
If you’re prescribed Cleocin, ask questions. If you’ve had side effects before, speak up. Antibiotics are powerful tools, but they’re not harmless. Choosing the right one matters-not just for your immediate infection, but for your long-term gut health and resistance to future bugs.
Don’t assume the first antibiotic you’re given is the best one. Your body-and your future self-will thank you.
Is Cleocin stronger than amoxicillin?
Cleocin (clindamycin) isn’t necessarily "stronger"-it’s just different. Amoxicillin works well against common bacteria like strep and some staph, but it doesn’t cover anaerobic bacteria as well. Cleocin fills that gap. For simple infections like strep throat or ear infections, amoxicillin is preferred. For deep abscesses or infections with anaerobic involvement, Cleocin may be more effective. Strength depends on the bug, not the drug.
Can I take doxycycline instead of Cleocin for acne?
Yes, doxycycline is actually the first-line oral antibiotic for moderate to severe acne, not Cleocin. It’s cheaper, has fewer side effects, and is just as effective. Cleocin is usually only used if doxycycline doesn’t work or if you can’t take it due to sun sensitivity or other reasons.
Is metronidazole better than Cleocin for bacterial vaginosis?
Metronidazole is the standard first treatment for bacterial vaginosis, not Cleocin. Studies show it clears the infection faster and with fewer side effects. Cleocin is only used if metronidazole doesn’t work or causes too much nausea. The vaginal gel form of metronidazole is often preferred because it avoids systemic side effects.
Why does Cleocin cause diarrhea?
Cleocin kills off a lot of good bacteria in your gut, especially in the colon. This lets harmful bacteria like Clostridioides difficile take over and produce toxins that cause inflammation and severe diarrhea. It’s not just "stomach upset"-it’s a serious imbalance that can require hospital treatment.
Are there natural alternatives to Cleocin?
No reliable natural substitute exists for treating bacterial infections like those Cleocin is used for. Garlic, honey, or tea tree oil might help with minor skin irritation, but they can’t replace antibiotics for infections like abscesses, cellulitis, or dental infections. Delaying proper treatment can lead to dangerous complications like sepsis.
How long does it take for Cleocin to work?
Most people start feeling better within 2-3 days if the infection is responding. But you must finish the full course-even if you feel fine. Stopping early can lead to the infection coming back or bacteria becoming resistant. If you don’t feel better after 3 days, call your doctor. The infection might need a different antibiotic.




Jenni Waugh
October 30, 2025 AT 15:44Oh wow, another doctor who thinks clindamycin is magic because it sounds fancy. Let me guess-your ‘specialized’ antibiotic is just the lazy fallback because your EHR auto-populates it? I’ve seen patients end up in the ER with C. diff because someone didn’t bother to check if amoxicillin-clavulanate would’ve worked. Stop prescribing like it’s 2008.
Theresa Ordonda
November 1, 2025 AT 03:19OMG I CANNOT BELIEVE THIS POST ISN’T VIRAL 😭 I had C. diff after 5 days of Cleocin for a tooth abscess. I was in pain for MONTHS. My gut felt like a war zone. Doxycycline? YES PLEASE. Metronidazole? I’d take that over Cleocin any day. Also, why is this still even a thing?? 🤦♀️💔
Judy Schumacher
November 1, 2025 AT 17:27While the comparative efficacy data presented herein is largely empirically sound, one must not overlook the confounding variables inherent in outpatient antibiotic prescription patterns. The 2024 analysis referenced, while statistically significant, fails to account for regional prescribing norms, physician training biases, and the influence of pharmaceutical marketing. Furthermore, the assertion that clindamycin is ‘not the universal solution’ is both trite and underwhelming-what is truly needed is a systemic overhaul of antibiotic stewardship protocols, not merely a substitution of one agent for another. The root issue lies not in the drug, but in the epistemological framework of contemporary primary care.
Megan Raines
November 2, 2025 AT 02:15So… you’re telling me the antibiotic I got for my wisdom tooth extraction wasn’t the best choice? Huh. Guess I’ll just add ‘learned the hard way’ to my resume. 😅
Mamadou Seck
November 3, 2025 AT 13:01Man I took Cleocin once and my stomach went full apocalypse. I switched to doxycycline for my acne and boom no more hellmouth. Why does everyone still use this thing like its a relic from the stone age
Anthony Griek
November 4, 2025 AT 11:23Just wanted to say thank you for laying this out so clearly. I’ve been fighting with my doctor to switch from Cleocin to cephalexin for my cellulitis, and honestly I felt like I was being difficult. But now I feel armed with facts. This is the kind of info we need more of.
Norman Rexford
November 4, 2025 AT 18:04Look i dont know why people are mad about cleocin i mean its american made right? and we got the best doctors here so if they prescribe it its prob the best. Plus i got a cousin who took it and he said it worked fine. dont let these science bros scare you. also doxycycline is for hippies anyway
Wayne Keller
November 5, 2025 AT 16:42Good breakdown. If you’re prescribed Cleocin, ask if there’s a safer option first. Most doctors are happy to explain. And if you’ve had diarrhea after antibiotics before? Say so. Your gut health matters more than you think. Don’t just take what’s handed to you.
Shana Labed
November 6, 2025 AT 09:06YESSSSSSS I’M SO GLAD THIS EXISTS. I had to beg my dentist to switch me from Cleocin to metronidazole for my abscess-I told him I’d rather risk the metallic taste than end up in the hospital with C. diff. He finally caved. Best decision ever. Also, probiotics? Non-negotiable. I take them like candy now. Your gut is your second brain, people. Treat it like it matters.
California Daughter
November 7, 2025 AT 17:17…but what if… you just… didn’t need antibiotics at all? 🤔 I mean, maybe the infection would’ve cleared on its own? Or maybe it wasn’t bacterial? Or maybe… we’re overprescribing everything? 🌿✨