MAOI Safety Checker
Drug Interaction Checker
Check safe washout periods between antidepressants and MAOIs based on clinical guidelines
Dietary Restrictions Checker
Check food safety based on your MAOI type
Food Risk Assessment
When you’ve tried multiple antidepressants and nothing works, your doctor might mention MAOIs. These aren’t your typical pills. They’re older, more powerful, and come with serious rules. But for some people with treatment-resistant depression, they’re the only thing that helps. The problem? Mixing them with other antidepressants can be deadly. And most doctors don’t know how to do it safely.
What Are MAOIs, Really?
Monoamine oxidase inhibitors - or MAOIs - were the first antidepressants ever made. Iproniazid, the first one, was originally an anti-tuberculosis drug. In the 1950s, doctors noticed patients on it started feeling happier. That’s how psychiatry got its first real chemical tool for depression. Today, you’ll still see them under brand names like Nardil (phenelzine), Parnate (tranylcypromine), and Emsam (selegiline patch). The patch version is newer and less restrictive - you don’t need to avoid all cheese if you’re on the low dose. But the older pills? They demand strict rules. MAOIs work by stopping your body from breaking down serotonin, norepinephrine, and dopamine. That means more of these mood-lifting chemicals hang around in your brain. For people with atypical depression - the kind where you feel heavy, sleep too much, and are hypersensitive to rejection - MAOIs often work when SSRIs fail. Studies show 40-60% of treatment-resistant patients respond to them.The Deadly Mix: MAOIs and SSRIs/SNRIs
The biggest danger? Combining MAOIs with SSRIs like fluoxetine (Prozac), sertraline (Zoloft), or SNRIs like venlafaxine (Effexor). This isn’t just risky - it’s life-threatening. This combo can trigger serotonin syndrome. Your body gets flooded with serotonin. Symptoms include high fever, rigid muscles, fast heart rate, confusion, and seizures. In severe cases, it kills. A 1995 study in the Journal of Clinical Psychiatry found that 7 out of 8 people who took fluoxetine and tranylcypromine together died. The FDA says it’s a hard no. You must wait at least 14 days after stopping any SSRI before starting an MAOI. But if you were on fluoxetine? Wait five weeks. Why? Fluoxetine and its active metabolite stick around in your system way longer than other SSRIs. Jumping in too soon means your body still has too much serotonin-blocking activity - and adding an MAOI pushes you over the edge.What About Tricyclic Antidepressants (TCAs)?
Here’s where things get messy. Most guidelines say: don’t mix MAOIs with TCAs like amitriptyline or clomipramine. But the reality is more nuanced. Clomipramine? Never combine it with MAOIs. It’s a strong serotonin reuptake blocker, and the risk is too high. But nortriptyline? That’s different. A 2009 study from the University of Pennsylvania tracked 56 treatment-resistant patients on phenelzine plus nortriptyline. Over half responded - with minimal side effects. The key? You must start the TCA first, or start both at the same time. Never add the MAOI after the TCA. That’s when things go wrong. A 2022 review in PMC noted that many doctors overestimate the danger. The fear comes from old case reports and theoretical models. Real-world data shows some combinations can be safe - if done right, slowly, and with close monitoring.Safe Alternatives: What You Can Combine
You don’t have to give up on combination therapy. There are antidepressants that play nice with MAOIs.- Bupropion (Wellbutrin): It doesn’t touch serotonin. It works on dopamine and norepinephrine. No serotonin syndrome risk. Many clinicians use it with MAOIs for low energy and lack of motivation.
- Mirtazapine (Remeron): This one boosts norepinephrine and serotonin in a different way - not by blocking reuptake. It’s been safely used with MAOIs in multiple case studies, especially for sleep and appetite issues.
- Trazodone: Often used for sleep, it’s also a mild antidepressant. It’s low-risk with MAOIs, especially at night doses.
- Nortriptyline: As mentioned, this TCA can work - but only if introduced correctly.

Dietary Rules Still Apply
MAOIs don’t just interact with drugs. They react with food. Tyramine - found in aged cheese, cured meats, tap beer, soy sauce, and fermented foods - can cause a sudden, dangerous spike in blood pressure. That’s a hypertensive crisis. It can lead to stroke or heart attack. If you’re on phenelzine or tranylcypromine, avoid:- Aged cheeses (like cheddar, blue cheese, parmesan)
- Tap beer and homebrewed alcohol
- Salami, pepperoni, and other fermented sausages
- Soym sauce, miso, and fermented tofu
Stopping MAOIs Isn’t Easy
You can’t just quit. Abruptly stopping MAOIs causes a withdrawal syndrome that feels like the flu - but worse. Symptoms include:- Restlessness (62% of cases)
- Upset stomach (48%)
- Tingling or burning skin (37%)
- Flu-like symptoms (55%)
- Severe insomnia (71%)
- Headaches (68%)
Why Aren’t More Doctors Prescribing Them?
MAOIs are effective. But they’re underused. Only 5-10% of depression specialists regularly prescribe them. Why? Fear. Lack of training. Outdated guidelines. A 2019 study found only 32% of psychiatry residents felt confident managing MAOIs. Most learned about them in textbooks, not in clinics. They’ve been painted as dangerous relics - when they’re actually powerful tools for the right patient. The real issue isn’t the drugs. It’s the system. Doctors aren’t taught how to use them safely. Patients aren’t told the full story. And that leaves people suffering.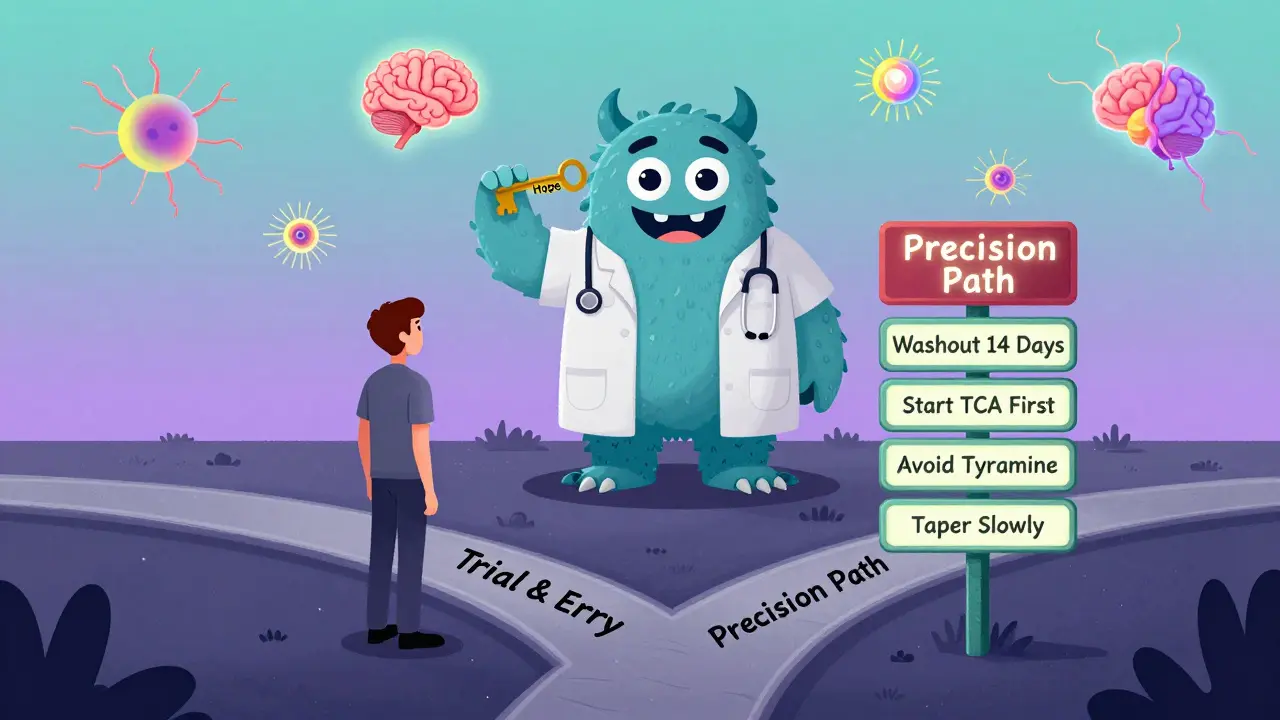
What’s Next for MAOIs?
Newer versions are coming. Selective MAO-B inhibitors are being studied to reduce side effects. There’s early research combining MAOIs with ketamine for rapid relief in treatment-resistant cases. But right now, the best path forward is simple: if you’ve tried two or more antidepressants and still feel stuck, ask about MAOIs. Not as a last resort - as a legitimate option. Find a doctor who knows how to use them. Someone who understands washout periods, safe combinations, and dietary needs. Don’t settle for guesswork. Your brain deserves precision, not trial and error.Frequently Asked Questions
Can I take an SSRI after stopping an MAOI?
Yes - but only after a proper washout. For most SSRIs, wait 14 days after your last MAOI dose. If you were on fluoxetine (Prozac), wait five weeks because it and its metabolite stay in your system much longer. Jumping in too soon can trigger serotonin syndrome, which can be fatal.
Is it safe to combine MAOIs with bupropion or mirtazapine?
Yes. Bupropion doesn’t affect serotonin reuptake, so it doesn’t raise serotonin syndrome risk. Mirtazapine works differently than SSRIs - it’s been safely used with MAOIs in clinical practice for treatment-resistant depression. Both are considered safe alternatives when used under supervision.
Why is clomipramine dangerous with MAOIs but nortriptyline isn’t?
Clomipramine is a strong serotonin reuptake inhibitor - it blocks serotonin from being cleared from the brain. When combined with an MAOI, which stops serotonin from breaking down, you get a dangerous flood of serotonin. Nortriptyline is weaker on serotonin and stronger on norepinephrine. Studies show it can be used safely with MAOIs if introduced correctly - not added after, but started at the same time or first.
Do I have to avoid all cheese on MAOIs?
Not always. The transdermal selegiline patch (Emsam) at 6mg/24hr doesn’t require dietary changes. But for oral MAOIs like phenelzine or tranylcypromine, avoid aged cheeses (cheddar, blue, parmesan), fermented meats, tap beer, and soy sauce. Tyramine in these foods can cause a dangerous spike in blood pressure. Always check your specific medication’s guidelines.
What happens if I stop an MAOI suddenly?
Stopping abruptly can cause withdrawal symptoms like restlessness (62% of cases), upset stomach, tingling skin, flu-like feelings, severe insomnia, and headaches. These aren’t just discomforts - they can be debilitating. Always taper slowly over 2-4 weeks under a doctor’s care to avoid this.
Are MAOIs still used today, or are they outdated?
They’re not outdated - they’re underused. MAOIs remain the most effective option for about 15-20% of people with treatment-resistant depression. Studies show 40-60% response rates where other drugs failed. The issue isn’t the drug - it’s that many doctors lack training in how to use them safely. For the right patient, they’re a lifeline.
Next Steps
- If you’re on an SSRI and thinking about switching to an MAOI: talk to your doctor about the 14- to 30-day washout period.
- If you’re considering combining an MAOI with another antidepressant: ask which ones are safe - and make sure your doctor knows the correct sequence.
- If you’re prescribed an MAOI: get a clear list of foods to avoid and a written tapering plan for when you stop.
- If you’ve tried multiple antidepressants without success: don’t assume there’s nothing left. Ask about MAOIs - specifically, ask if you’re a candidate for treatment-resistant depression protocols.





Jay Tejada
January 4, 2026 AT 19:22Man, I wish my doc knew half as much as this post. I was on Zoloft for years until I nearly turned into a human toaster. Now I’m on Emsam and actually sleep through the night. Cheese? Still scared of it. But hey, I’m alive and not crying in the shower every morning.
Stephen Craig
January 6, 2026 AT 16:34MAOIs aren’t dangerous. They’re just misunderstood. Most doctors treat them like nuclear weapons because they were never taught how to handle them. The real tragedy is patients suffering because of ignorance, not the medication.
Connor Hale
January 8, 2026 AT 15:49This is one of the clearest, most humane explanations of MAOIs I’ve ever read. It’s not about fear - it’s about precision. Too many people are told there’s nothing left when the truth is they just haven’t found the right tool yet.
Justin Lowans
January 9, 2026 AT 12:06As someone who’s worked in psychopharmacology for over two decades, I can say with confidence that this post is a masterclass in clinical nuance. The distinction between clomipramine and nortriptyline alone deserves to be printed in every residency handbook. Thank you for articulating what so many of us see daily but rarely get to say aloud.
Michael Rudge
January 11, 2026 AT 07:24Wow. Another one of those ‘I read one paper and now I’m a psychiatrist’ posts. Did you also invent the concept of serotonin? Maybe you should write a textbook while you’re at it - I’m sure your 14-year-old Reddit research qualifies you.
Cassie Tynan
January 12, 2026 AT 16:49Michael, you’re the reason people don’t trust doctors. You think sarcasm makes you smart? Nah. It just makes you the guy who yells at the weatherman because it didn’t predict his existential crisis. This post saved lives. Shut up and read it again.
Vikram Sujay
January 14, 2026 AT 07:26There is a profound ethical responsibility in prescribing psychopharmacological agents that alter the fundamental chemistry of consciousness. The historical neglect of MAOIs reflects not a failure of pharmacology, but a failure of medical education to honor the complexity of human neurobiology. To dismiss them as relics is to misunderstand the nature of progress - which is not the replacement of old tools, but the refinement of their application. This post, in its meticulousness, restores dignity to a therapeutic tradition that has been unjustly vilified by fear and inertia.
Rory Corrigan
January 15, 2026 AT 02:54bro this is so deep 😭 i’ve been on nardil for 3 years and now i get it… serotonin is like a cosmic river and we’re just trying to build dams with our minds 🌊🧠