Menstrual Cycle Hormone Tracker
This interactive tool shows how hormone levels change throughout the menstrual cycle. Click on any phase to see detailed information.
Menstrual Phase
Days 1-5
FSH: 5-10 IU/LLH: 2-5 IU/L
Estradiol: 30-80 pg/mL
Progesterone: 0.1-0.5 ng/mL
Follicular Phase
Days 6-13
FSH: 8-12 IU/LLH: 4-8 IU/L
Estradiol: 80-150 pg/mL
Progesterone: 0.2-0.8 ng/mL
Ovulation
Day 14
FSH: 5-9 IU/LLH: 30-100 IU/L
Estradiol: 300-500 pg/mL
Progesterone: 1-2 ng/mL
Luteal Phase
Days 15-28
FSH: 5-8 IU/LLH: 5-10 IU/L
Estradiol: 100-200 pg/mL
Progesterone: 5-20 ng/mL
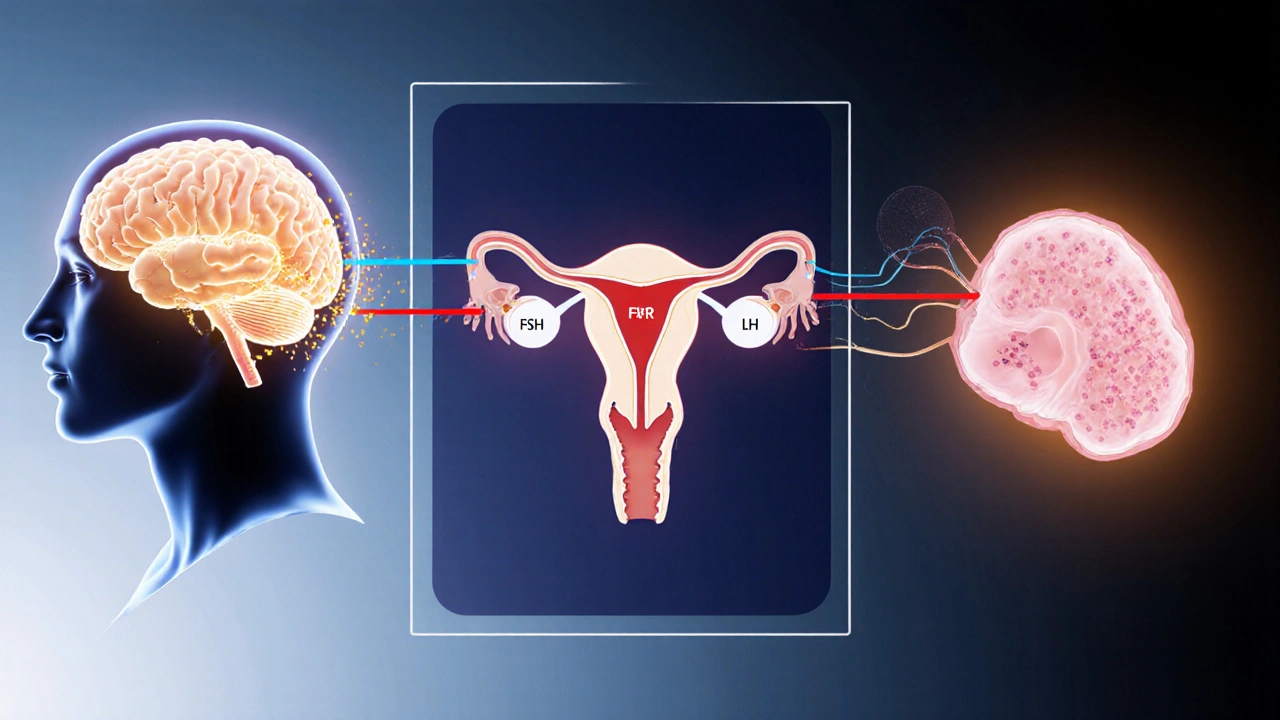
Hormone Feedback Loops
Negative Feedback
High estrogen or progesterone signals the hypothalamus and pituitary to reduce GnRH, FSH, and LH production to prevent premature ovulation or over-stimulation.
Positive Feedback
When estradiol peaks, it triggers the LH surge. This short-lived loop is the only situation where higher hormone levels stimulate more release.
Key Hormone Functions
FSH
Drives early follicle recruitment and estrogen production.
LH
Triggers ovulation and supports corpus luteum function.
Estrogen
Promotes follicle growth and prepares uterine lining.
Progesterone
Stabilizes uterine lining for possible implantation.
GnRH
Hypothalamic signal that prompts pituitary release of FSH and LH.
Understanding how the body times ovulation and the monthly bleed can feel like trying to read a code written in a foreign language. The good news is that the hormonal control of ovulation follows a predictable pattern, driven by a handful of key chemicals and the brain‑ovary communication loop. Below is a plain‑English walk‑through of the players, the phases, and the feedback loops that keep the cycle in sync.
Key Takeaways
- The hypothalamus, pituitary gland, and ovaries form the H‑P‑O axis that drives the menstrual cycle.
- Follicle‑stimulating hormone (FSH) and luteinizing hormone (LH) are the main triggers for follicle growth and egg release.
- Estrogen peaks in the late follicular phase, while progesterone dominates the luteal phase.
- Negative and positive feedback loops create the LH surge that initiates ovulation.
- Disruptions in any hormone can lead to irregular cycles, anovulation, or amenorrhea.
1. The Hypothalamus‑Pituitary‑Ovary (H‑P‑O) Axis
At the top of the control tower sits the hypothalamus is a small brain region that secretes gonadotropin‑releasing hormone (GnRH) to start the cascade. GnRH travels a short distance to the pituitary gland is the master endocrine organ that releases FSH and LH into the bloodstream. These two hormones reach the ovaries, where they tell follicles when to grow, mature, and finally release an egg. Think of the axis as a three‑person relay race: the hypothalamus hands the baton to the pituitary, which then hands it to the ovary.
2. The Main Hormone Players
Each hormone has a clear job, but their levels rise and fall like a tide.
- Follicle‑stimulating hormone (FSH) is the driver of early follicle recruitment and estrogen production.
- Luteinizing hormone (LH) is the spark that triggers ovulation and later supports the corpus luteum.
- Estrogen is a group of hormones (mainly estradiol) that promote follicle growth and prepare the uterine lining.
- Progesterone is the hormone that stabilises the uterine lining for possible implantation.
- Gonadotropin‑releasing hormone (GnRH) is the hypothalamic signal that makes the pituitary release FSH and LH.
3. Follicular Phase - From Menstruation to the Estrogen Surge
Day1 of the cycle is marked by the first day of menstruation is the shedding of the previous cycle’s uterine lining. As bleeding tapers, the hypothalamus releases low‑dose GnRH pulses, prompting the pituitary to secrete a modest amount of FSH. These FSH molecules travel to the ovaries, waking up a cohort of antral follicles.
Inside each follicle, granulosa cells start converting androgens (from the theca cells) into estradiol - the primary form of estrogen. Rising estrogen does two things: it thickens the endometrium and, via a negative feedback loop, tells the pituitary to ease off FSH production, preventing too many follicles from maturing at once.
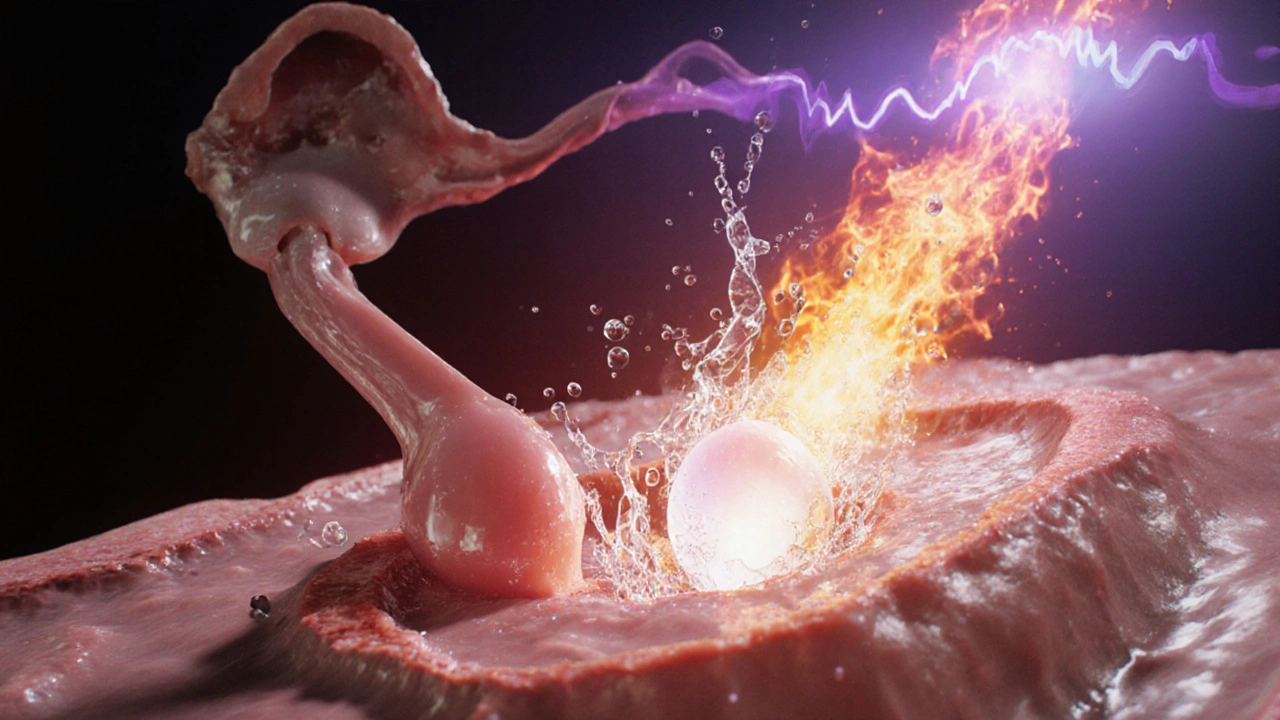
4. The LH Surge - How Ovulation Happens
When estradiol reaches a critical threshold (usually around day12‑14 in a 28‑day cycle), the feedback flips from negative to positive. The hypothalamus suddenly ramps up GnRH pulse frequency, which pushes the pituitary to dump a massive LH pulse - the famed LH surge.
This surge does the heavy lifting: the dominant follicle ruptures, spilling its mature oocyte into the fallopian tube. Simultaneously, the follicle cells start turning into the corpus luteum is a temporary endocrine structure that secretes progesterone and some estrogen.
5. Luteal Phase - Progesterone Takes the Lead
After ovulation, the corpus luteum churns out progesterone (and a bit of estrogen). Progesterone tells the uterine lining to become “secretory” - rich, nutrient‑filled, and ready for an embryo. If fertilisation does not occur, the corpus luteum involutes around day22‑24, causing progesterone and estrogen to fall sharply.
The hormone drop removes the inhibitory signal on the hypothalamus, allowing the GnRH‑FSH‑LH cycle to restart and the uterus to shed its built‑up lining - the next menstrual bleed.
6. Quick Reference: Hormone Levels Across Cycle Phases
| Phase | FSH (IU/L) | LH (IU/L) | Estradiol (pg/mL) | Progesterone (ng/mL) |
|---|---|---|---|---|
| Menstrual (Days1‑5) | 5‑10 | 2‑5 | 30‑80 | 0.1‑0.5 |
| Early Follicular (Days6‑9) | 8‑12 | 4‑8 | 80‑150 | 0.2‑0.8 |
| Late Follicular (Days10‑13) | 6‑10 | 6‑10 | 200‑350 | 0.5‑1.0 |
| Ovulation (Day14) | 5‑9 | 30‑100 (surge) | 300‑500 | 1‑2 |
| Luteal (Days15‑28) | 5‑8 | 5‑10 | 100‑200 | 5‑20 (peak days21‑23) |
7. Feedback Loops - The Body’s Self‑Correcting System
Two loops keep everything on schedule:
- Negative feedback - High estrogen or progesterone signals the hypothalamus and pituitary to tone down GnRH, FSH, and LH production. This prevents premature ovulation or over‑stimulation of the ovaries.
- Positive feedback - When estradiol peaks, it flips the switch, causing the LH surge. This short‑lived positive loop is the only hormonal situation in the menstrual cycle where higher levels stimulate more release.
If either loop misfires, you get conditions like anovulatory cycles (no LH surge) or luteal phase defects (insufficient progesterone).
8. Common Disruptions and When to Seek Help
Understanding the hormone timeline helps spot problems early.
- Polycystic ovary syndrome (PCOS) - Excessive early‑phase LH relative to FSH, leading to many small follicles and irregular ovulation.
- Hypothalamic amenorrhea - Low GnRH output caused by stress, weight loss, or excessive exercise; results in low FSH/LH and absent periods.
- Luteal phase defect - Inadequate progesterone production; may cause early spotting or trouble sustaining early pregnancy.
Blood tests that measure FSH, LH, estradiol, and progesterone on specific cycle days can pinpoint where the disruption lies. Treatment usually targets the underlying feedback issue - for example, metformin for PCOS or lifestyle changes for hypothalamic amenorrhea.

Frequently Asked Questions
Why does the LH surge happen only once per cycle?
The surge is triggered by a brief window of positive estradiol feedback. Once estrogen drops after ovulation, the feedback returns to negative, shutting down the surge mechanism until the next cycle.
Can I track my hormone levels at home?
Several over‑the‑counter kits measure LH in urine (the classic “ovulation test”) and some now offer estrogen or progesterone strips. For precise values, a blood draw ordered by a clinician is still the gold standard.
What causes a missed period if I’m not pregnant?
Common culprits include stress‑induced low GnRH, rapid weight change, thyroid imbalance, or conditions like PCOS that disrupt the normal hormone rhythm.
How long does the corpus luteum survive without fertilisation?
Typically 10‑14days. If pregnancy occurs, it transforms into the placenta and continues progesterone production.
Is it possible to have a normal cycle without estrogen?
No. Estrogen is essential for follicle maturation and building the uterine lining. Very low estrogen typically results in amenorrhea and infertility.
Why do some women experience spotting after ovulation?
Mild estrogen drops or a brief luteal phase progesterone dip can cause tiny blood vessels in the endometrium to break, leading to light spotting. It’s usually harmless if it’s brief.





Stu Davies
October 4, 2025 AT 13:28Wow, that overview breaks the cycle down nicely 😊. It’s like having a cheat sheet for the whole month.
bruce hain
October 10, 2025 AT 08:22While comprehensive, the article could benefit from citing primary endocrine studies.
Sukanya Borborah
October 16, 2025 AT 03:15Honestly, the section on “positive feedback” is riddled with redundant phrasing and the term “hormone feedback loops” should be singular when referring to the specific LH surge mechanism; also, “is a small brain region” lacks proper article usage.
Greg RipKid
October 21, 2025 AT 22:08Pretty solid summary, gets the main players across without drowning you in biochemistry.
Nadia Stallaert
October 27, 2025 AT 16:02When diving into the hormonal symphony of the menstrual cycle, one cannot help but notice the intricate choreography that rivals any grand ballet; the hypothalamus initiates the performance with GnRH pulses that echo through the pituitary, releasing FSH and LH in a precisely timed duet. The follicular phase emerges like a crescendo, with estrogen climbing steadily, painting the uterine lining in soft pastels while simultaneously fine‑tuning the feedback loops that keep the system from spiraling out of control. As estrogen peaks, the narrative flips, and a sudden LH surge bursts forth, akin to a dramatic climax that forces the dominant follicle to rupture and release its egg onto the stage of the fallopian tube. The corpus luteum then takes center stage, producing progesterone that transforms the endometrium into a lush, secretive garden ready for implantation, a role reminiscent of a nurturing caregiver. Yet, if fertilization does not occur, the luteal curtain falls, progesterone wanes, and the cycle resets, allowing the next act to begin anew. Throughout this drama, negative feedback acts as a vigilant director, quietly reminding the hypothalamus and pituitary to tone down hormone production, while positive feedback appears only briefly, like a spotlight that highlights the LH surge. Disruptions in any of these cues can lead to conditions that feel like plot twists in a poorly written novel, such as anovulatory cycles or luteal phase defects, each demanding careful clinical attention. Moreover, external factors like stress, extreme exercise, or nutritional deficiencies can hijack the GnRH pulse generator, leading to hypothalamic amenorrhea-a storyline where the script is abruptly halted. Understanding the hormonal timeline empowers both clinicians and individuals to anticipate irregularities, interpret symptoms, and perhaps intervene with therapies that restore balance, whether through lifestyle adjustments or pharmacologic agents. In practice, tracking basal body temperature, cervical mucus, or using ovulation predictor kits can provide tangible clues that align with the underlying endocrine fluctuations. It is also fascinating to note that modern wearable technology now attempts to infer hormone levels indirectly, offering a glimpse into this hidden world. Ultimately, the menstrual cycle exemplifies a masterpiece of endocrine engineering, where each hormone plays its part with exquisite precision, guided by feedback loops that ensure harmony and continuity. By appreciating this complexity, we move beyond seeing the cycle as merely a monthly inconvenience and recognize it as a dynamic, adaptive system essential to reproductive health. Researchers continue to unravel micro‑RNA and epigenetic influences that modulate each phase, hinting at even deeper layers of regulation. Future therapies may target these subtle pathways, offering hope for those with refractory cycle disorders.
John Price Hannah
November 2, 2025 AT 10:55And yet, the so‑called “scientific consensus” you glorify is nothing but a façade-an orchestrated narrative designed to keep the masses in hormonal complacency!!!
Elle McNair
November 8, 2025 AT 05:48I see both sides and just think the info is useful
Dennis Owiti
November 14, 2025 AT 00:42Thats great, but maybe add a bit more on how stress affects GnRH selcction.
Michael Christian
November 19, 2025 AT 19:35Love how the chart makes the hormone swings visual-great tool for anyone trying to sync their cycle.
Steven Elliott
November 25, 2025 AT 14:28Sure, because a table is going to solve everyone's irregular cycles, right?
Cameron White
December 1, 2025 AT 09:22What they don’t tell you is how pharma uses this data to push synthetic hormones on us all the time.
Amélie Robillard
December 7, 2025 AT 04:15Finally, a digestible guide! 🌟 Keep these coming.
Fae Wings
December 12, 2025 AT 23:08✨Your enthusiasm is contagious; I can already feel the rhythm aligning in my soul! 😍
Anupama Pasricha
December 18, 2025 AT 18:02Indeed, the integration of GnRH pulsatility with peripheral feedback loops forms a highly synchronized endocrine axis, and understanding this framework can optimize both clinical interventions and personal tracking.
Bryce Charette
December 24, 2025 AT 12:55Nice job, but watch out for “the corpus luteum churns out progesterone” – it should be “churns out progesterone” without extra “the”.
Christina Burkhardt
December 30, 2025 AT 07:48Thanks for the tip! I’ll keep an eye on those articles when I edit next time.
Echo Rosales
January 5, 2026 AT 02:42Honestly, all this hormone talk feels overhyped.