Most women don’t realize that the critical window for fetal development begins before they even know they’re pregnant. By week 3, the neural tube - which becomes the brain and spine - is already forming. By week 8, the heart, limbs, and organs are taking shape. If you’re taking any medication - prescription, over-the-counter, or even herbal - and you’re planning to conceive, waiting until you miss your period to check if it’s safe is too late. That’s why creating a medication plan before conception isn’t just smart - it’s essential.
Why Timing Matters More Than You Think
The first eight weeks of pregnancy are the most dangerous for medication exposure. This is when the baby’s body is building its foundation. By the time most women take a pregnancy test, they’re already six weeks along. And according to the American College of Obstetricians and Gynecologists (ACOG), nearly half of all pregnancies in the U.S. are unplanned. That means millions of women are unknowingly exposing their developing babies to risks every month. You might think, “I’m healthy, I don’t take anything dangerous.” But here’s the catch: common medications like ibuprofen, certain acne treatments, and even some supplements can carry hidden risks. The key isn’t avoiding all meds - it’s knowing which ones need to be switched, stopped, or adjusted before you start trying.Start with a Full Medication Inventory
Before you even talk to a doctor, write down everything you’re taking. Not just prescriptions. Include:- All prescription drugs (even if you’ve been on them for years)
- Over-the-counter painkillers, cold meds, and sleep aids
- Vitamins, herbal supplements, and CBD products
- Topical creams and patches (like nicotine or hormone patches)
Folic Acid: The One Supplement That Can’t Be Skipped
Folic acid is the only supplement with overwhelming, proven evidence for preventing birth defects - specifically neural tube defects like spina bifida. The World Health Organization recommends 400 mcg daily for all women aged 15 to 49, regardless of pregnancy plans. But if you have certain conditions, you need more.- General population: 400-800 mcg per day
- Women with epilepsy on valproic acid: 4-5 mg per day
- Women with diabetes, obesity, or a previous affected pregnancy: 4 mg per day
Medications That Must Be Changed Before Pregnancy
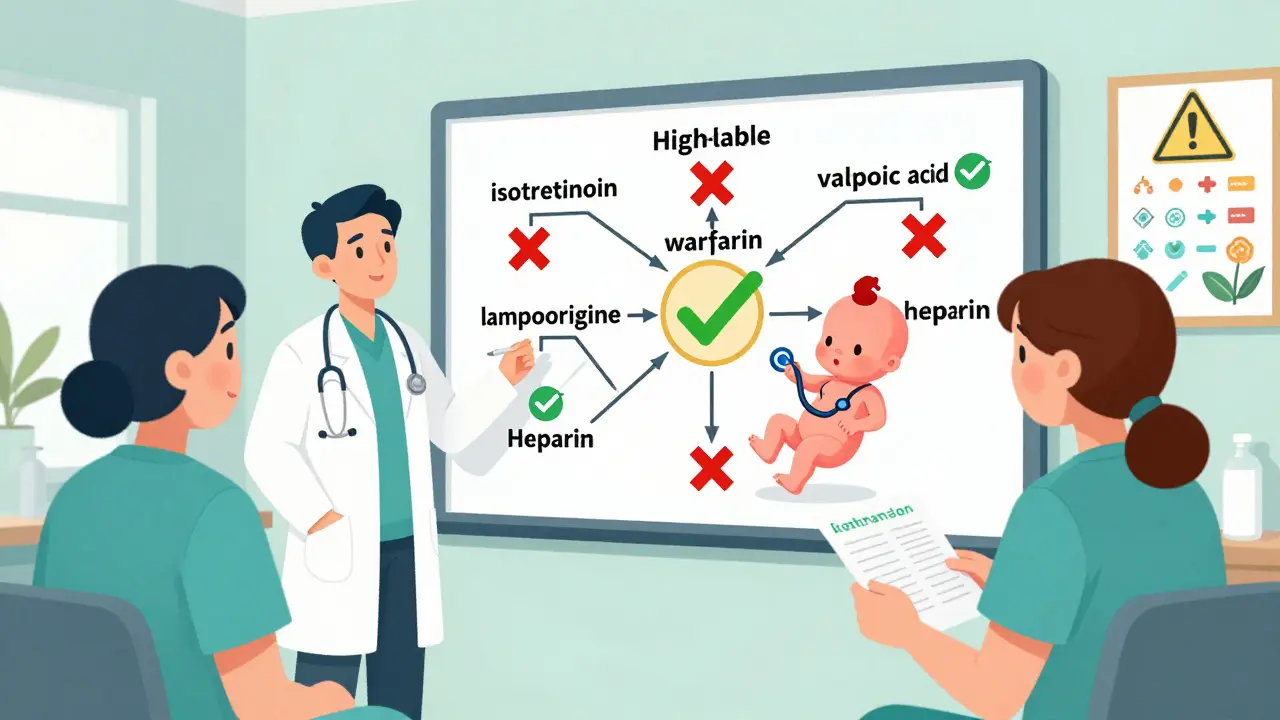
Some drugs are known to cause serious birth defects. These aren’t “maybe risky” - they’re well-documented dangers.- Valproic acid (for seizures or bipolar): Linked to a 10.7% rate of major birth defects. Switch to lamotrigine or levetiracetam if possible.
- Lithium (for bipolar disorder): Increases risk of Ebstein’s anomaly (a heart defect) by 1 in 2,000 births. Requires careful monitoring and possible switch.
- Methotrexate (for autoimmune diseases or cancer): Causes miscarriage and severe malformations. Must be stopped at least 3 months before conception.
- Isotretinoin (Accutane for acne): Causes severe skull, heart, and brain defects. You must wait one full month after stopping before trying to conceive.
- Warfarin (blood thinner): Crosses the placenta and causes fetal warfarin syndrome. Switch to heparin injections before pregnancy.
- Topiramate (for seizures or migraines): Doubles the risk of cleft lip or palate.
Managing Chronic Conditions Before Pregnancy
If you have a long-term health condition, your preconception plan isn’t just about stopping bad meds - it’s about optimizing your health.- Thyroid disease: Your TSH level should be under 2.5 mIU/L before conception. Once pregnant, your levothyroxine dose will need to increase by about 30%. Waiting until pregnancy to adjust can raise miscarriage risk by 60%.
- High blood pressure: ACE inhibitors and ARBs are dangerous in pregnancy. Switch to labetalol, nifedipine, or methyldopa.
- Diabetes: Aim for an HbA1c below 6.5% before trying. High blood sugar in early pregnancy increases the risk of heart defects and miscarriage.
- Autoimmune diseases (lupus, rheumatoid arthritis): Avoid methotrexate and leflunomide. Sulfasalazine and hydroxychloroquine are generally safe. Work with a rheumatologist at least 4-8 weeks before conception.
- HIV: Your viral load must be below 50 copies/mL before conception. With proper treatment, transmission risk drops from 25% to under 1%.
What About Birth Control?
If you’re on hormonal birth control and planning to conceive, you don’t need to wait months after stopping. Ovulation usually returns within weeks. But here’s the catch: if you’re on seizure meds like carbamazepine or phenytoin, your birth control pills may not work. These drugs speed up how your body breaks down hormones. You might think you’re protected - but you’re not. Use a backup method - condoms or an IUD - while switching to safer meds. Don’t assume your pill is doing its job. Ask your doctor about non-hormonal options if you’re on enzyme-inducing drugs.When to See Who
You don’t need to see a specialist right away - but timing matters.- Primary care provider: Start here. Bring your medication list. They can flag red flags and refer you.
- Obstetrician or midwife: Schedule a preconception visit at least 3-6 months before trying. They’ll check your folic acid, blood pressure, and immunizations.
- Specialists: If you have epilepsy, see a neurologist. For autoimmune disease, see a rheumatologist. For mental health, work with your psychiatrist. These visits should happen 4-8 weeks before you plan to conceive.
What If You’re Already Pregnant?
If you’re already pregnant and haven’t reviewed your meds, don’t panic. But act fast. Call your doctor or midwife immediately. Some medications can still be switched safely in early pregnancy. Folic acid can still help if you start now. And if you’re on something dangerous, your provider can monitor for complications with ultrasounds and blood tests. The goal isn’t guilt - it’s action. You’re not behind. You’re just starting.What’s Stopping People From Doing This?
Only 24% of OB/GYNs in the U.S. consistently review medications before pregnancy, even though 89% say it’s important. Why? Time. Most appointments are 15 minutes. Many doctors don’t have access to up-to-date teratogen databases. And women often don’t know to ask. But you can change that. Bring your list. Ask: “Is anything I’m taking risky for pregnancy?” “What’s the safest alternative?” “Do I need to stop or switch anything?” If your provider doesn’t know, ask for a referral to a maternal-fetal medicine specialist or a preconception clinic.Final Checklist: Your Preconception Medication Plan
Use this before you stop birth control:- ☐ Written list of all medications (prescription, OTC, supplements)
- ☐ Started 400-800 mcg folic acid daily (4-5 mg if high-risk)
- ☐ Reviewed high-risk drugs: valproic acid, lithium, methotrexate, isotretinoin, warfarin
- ☐ Chronic conditions optimized: thyroid, blood pressure, diabetes, mental health
- ☐ Birth control method checked for drug interactions
- ☐ Scheduled preconception visit with OB/GYN or midwife
- ☐ Scheduled specialist visits (neurologist, rheumatologist, etc.) if needed
- ☐ Documented plan with your provider - ask for ICD-10 code Z31.69 to be recorded
Can I keep taking my antidepressants if I’m trying to get pregnant?
Some antidepressants are safer than others during pregnancy. SSRIs like sertraline and citalopram are generally considered low-risk. Avoid paroxetine - it’s linked to a small increase in heart defects. Never stop antidepressants cold turkey - that can trigger relapse, which is also dangerous for pregnancy. Work with your psychiatrist to switch to a safer option at least 2-3 months before conception.
Is it safe to take herbal supplements before pregnancy?
Many herbal supplements aren’t tested for safety in pregnancy. Black cohosh, dong quai, and high-dose vitamin A can be harmful. Even “natural” doesn’t mean safe. Stick to prenatal vitamins with folic acid and avoid anything not approved by your doctor. If you use supplements for anxiety, sleep, or hormones, bring them to your preconception visit.
How long should I wait after stopping a risky medication?
It depends on the drug. Methotrexate needs 3 months (3 full ovulatory cycles). Isotretinoin requires 1 month. Lithium and valproic acid can be switched immediately, but you need time to stabilize on the new drug. Always follow your provider’s timeline - don’t guess. Some drugs stay in your system longer than you think.
Do I need to see a specialist if I’m healthy?
If you’re healthy and only taking a daily multivitamin and occasional ibuprofen, you may not need a specialist. But if you’ve had surgery, chronic illness, mental health treatment, or take more than two medications, a preconception checkup is strongly recommended. Even healthy women benefit from folic acid guidance and a medication safety review.
What if my partner is taking medication?
Men’s medications can also affect fertility and embryo development. Some drugs like finasteride, sulfasalazine, or chemotherapy can lower sperm quality. While the risk to the baby is lower than maternal exposure, it’s still worth reviewing. If your partner is on any long-term medication, ask his doctor if it could impact conception or early development.






Gerard Jordan
January 20, 2026 AT 00:11Just read this and immediately sent the link to my girlfriend who’s been on birth control for 7 years and never thought to check her meds. 🙌 Folic acid alone is worth the 5 minutes it takes to read this. Seriously, why isn’t this standard info in every gynecologist’s waiting room?
Sangeeta Isaac
January 20, 2026 AT 10:38lol i thought i was being careful taking my ‘natural’ ashwagandha for stress… turns out it’s basically a hormone whisperer and i’ve been flirting with teratogenic territory for 2 years. thanks for the gut punch, internet. going to dump my supplement drawer into a bag labeled ‘what i thought was wellness’ and take it to my dr tomorrow. 🤦♀️
Ben McKibbin
January 21, 2026 AT 11:31This is one of the most clinically grounded, accessible, and necessary posts I’ve seen in years. The breakdown of valproic acid vs. lamotrigine? The specificity on folic acid dosing by condition? The inclusion of paternal medication risks? It’s not just informative-it’s a public health imperative. Someone should turn this into a CDC pamphlet. I’ve already shared it with three friends planning pregnancies. No fluff, no fearmongering-just evidence wrapped in plain speech. Thank you.
Melanie Pearson
January 22, 2026 AT 08:39Let’s be honest: this is just another example of medical overreach disguised as ‘precaution.’ If you’re healthy and not taking dangerous drugs, why are you being told to overhaul your entire life based on hypothetical risks? The WHO recommends folic acid for all women 15–49? That’s not prevention-it’s population control disguised as care. And now we’re supposed to consult six specialists before even trying to conceive? This isn’t medicine. It’s anxiety marketing.
Uju Megafu
January 23, 2026 AT 08:43OMG I can’t believe people are still taking ibuprofen before pregnancy?? Like, are you even trying?? My cousin had a baby with a cleft palate and they found out she was taking Advil every week for headaches. It’s not ‘maybe risky’-it’s a baby-destroying choice. And if you’re on antidepressants and think it’s ‘fine’-you’re just being selfish. Your child’s brain matters more than your comfort. Stop making excuses.
Andrew Rinaldi
January 24, 2026 AT 22:35I appreciate the intent behind this, but I wonder how many women feel paralyzed by it. I’m 32, on a low-dose SSRI for anxiety, take a daily multivitamin, and have no chronic conditions. Do I really need to swap my sertraline for a different one, just in case? What if the switch makes me worse? And who’s going to pay for the 4 specialist visits? This feels like a privilege checklist disguised as public health advice. I’m not ignoring safety-I’m just tired of being told I’m failing before I even start.
Dee Monroe
January 25, 2026 AT 06:14It’s funny how we treat conception like a science experiment instead of a natural process. I get the data, I do-I’ve read the ACOG guidelines, I know about neural tube closure and teratogens-but there’s something deeply human here that gets lost. We’re not just vessels for fetal development. We’re people with lives, histories, mental health, jobs, trauma, and joy. And yes, we should be informed-but we shouldn’t be guilt-tripped into becoming medical compliance robots. I took my folic acid for 6 months before trying. I switched my acne meds. I talked to my therapist. And then I got pregnant… and I didn’t stress about the occasional Advil I took before I knew. I’m not a statistic. I’m a mother. And I did the best I could with what I knew. That’s enough.
Philip Williams
January 27, 2026 AT 05:33For those questioning the necessity of preconception medication reviews: consider this. In 2022, the CDC reported that 1 in 33 infants in the U.S. is born with a major birth defect. A significant proportion of these are linked to medication exposure during the first trimester. Preconception planning is not overcautious-it is preventative medicine at its most effective. The cost of a single specialist consultation is negligible compared to the lifelong medical, emotional, and financial burden of managing a preventable congenital anomaly. This is not fear. This is responsibility.
Alex Carletti Gouvea
January 27, 2026 AT 07:10Why are we even talking about this? In my day, women just got pregnant and dealt with it. No lists. No specialists. No ‘folic acid this’ or ‘switch that.’ You took what you took and trusted God. Now we’ve turned motherhood into a bureaucratic nightmare. This post reads like a corporate compliance manual, not advice for real people. We’ve lost the simple faith that the body knows what to do.