Stop Throwing Away Good Medicine
You open the cabinet and find a bottle of pills you forgot about. The expiration date is next month. You think, Should I toss this? You’re not alone. Every year, clinics, pharmacies, and homes in New Zealand and around the world throw away millions of dollars worth of medicine that’s still safe and effective. The problem isn’t just money-it’s waste, environmental harm, and missed chances to help people who can’t afford prescriptions.
The good news? You don’t need fancy tech or a big budget to cut down on this waste. Real change starts with simple, smart habits.
Store Medicines Right-It’s Not Just About the Shelf
Most people think if a medicine is in a cupboard, it’s fine. But temperature and light matter more than you think.
Insulin, certain antibiotics, and biologics need to stay cold: between 2°C and 8°C. If they get too hot-even for a few hours-they lose effectiveness. That’s not speculation. A 2022 case in a rural clinic saw $8,200 in insulin go bad because the fridge broke and no one noticed for three days.
Room-temperature meds like blood pressure pills or antibiotics should stay between 20°C and 25°C. Don’t store them above the stove, in the bathroom, or in direct sunlight. A drawer in a cool bedroom is better than a medicine cabinet above the sink.
Use a small fridge thermometer for refrigerated meds. Check it every week. If it’s outside the range, act fast. Call your pharmacist. Don’t guess.
Use FIFO-It’s Not Just for Groceries
FIFO stands for First In, First Out. It’s a simple rule: use the oldest stock first. Sounds obvious? Most people don’t do it.
When a new box of pills arrives, put it behind the old one. Not in front. That way, the bottle with the earliest expiration date gets used first. This one habit alone can prevent 15-20% of waste in small clinics and households.
Make it part of your routine. Every Friday morning, take five minutes to check your medicine shelf. Move older bottles to the front. Put new ones in back. Use color-coded labels-red for meds expiring in 30 days, yellow for 60 days. It’s low-tech, but it works. Nurse Practitioner Elena Rodriguez cut her clinic’s waste by 29% using this method.

Don’t Over-Prescribe-Ask for Less
Doctors often give you a 30-day supply because it’s easier. But what if you only need 10 days? Or 14?
Dr. Sarah Thompson from Mayo Clinic says the single biggest way to reduce waste is to ask for smaller quantities. Especially for chronic conditions like thyroid meds or antidepressants. Instead of a 90-day supply, ask for 30. You can refill as needed.
This isn’t just about saving pills. It’s about safety. If your treatment plan changes, you won’t be stuck with unused meds. And if you forget to take them, you’re not hoarding a full bottle that might expire before you use it.
Pharmacists can split prescriptions. You don’t need to take the whole bottle. Just ask: “Can I get half the quantity this time?”
Track Expirations Like a Pro
Most people don’t know when their meds expire until they’re already past it. That’s too late.
Use a free app or a simple spreadsheet. List each medicine, its expiration date, and where it’s stored. Update it every time you refill. Set a calendar alert for 30 days before expiration. That way, you have time to use it-or return it.
For clinics: barcode scanners and cloud systems like Omnicell or Epic reduce waste by 22-30%. But you don’t need them. Even a printed checklist taped to the wall works. Just write down what you have and when it expires. Check it weekly.
Dispose of What You Can’t Use-Safely
Expired or unused meds shouldn’t go in the trash or down the drain. They end up in rivers, soil, and drinking water.
In New Zealand, the safest option is a take-back program. Many pharmacies, hospitals, and community centers offer free drop-off bins for old or unwanted medicines. The Ministry of Health supports these programs, and they’re available in over 90% of urban areas.
If you can’t find a drop-off point, mix pills with coffee grounds or cat litter in a sealed container. Throw that in the trash. Never flush unless it’s on the FDA’s “flush list”-which includes certain opioids. Most meds don’t belong in the toilet.
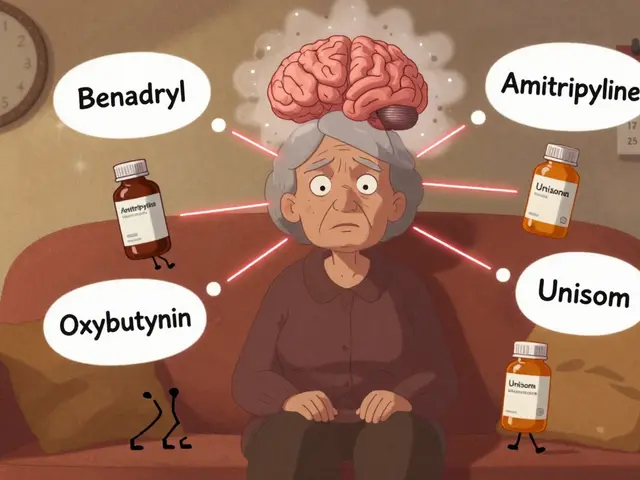
And never give your meds to someone else. Even if it’s the same condition. Dosing is personal. What works for you could harm someone else.

Think Twice About “Expiration” Dates
Here’s something most people don’t know: many medicines stay effective long after their printed expiration date.
A 2021 JAMA study found that 88% of tested drugs retained potency for years past their label date. The FDA’s own Shelf Life Extension Program shows some meds work fine 10-15 years later.
That doesn’t mean you should keep everything forever. But it does mean you shouldn’t panic when you see a date that’s a few months past. Check the pill’s appearance. Is it discolored? Crumbly? Smelling weird? If not, it’s probably still safe.
When in doubt, call your pharmacist. They can check stability data. Don’t toss it just because the date says so.
Small Steps, Big Impact
You don’t need to overhaul your life to make a difference. Start with one thing:
- Check your medicine cabinet this week. Find one bottle that’s about to expire.
- Use it-or take it to a drop-off point.
- Next time you get a prescription, ask for a smaller amount.
- Put the oldest meds in front.
- Set a calendar reminder for expiration dates.
These aren’t just good habits-they’re smart economics and environmental action. A 2021 study of 127 small clinics found that practices using these simple steps saved an average of $15,000 a year in wasted meds.
And when you reduce waste, you help others too. More medicine stays in the system. More people get what they need. Less ends up in landfills.
What’s Next?
The future of medication management is smarter tech-AI predicting usage, automated alerts, real-time tracking. But right now, the biggest gains come from the simplest actions: storing right, using first, asking for less, and disposing safely.
You don’t need to be a pharmacist or a hospital administrator to make this change. You just need to care enough to check one bottle. Then another. And another.
Can I still use medicine after the expiration date?
Many medicines remain safe and effective well past their printed expiration date, especially if stored properly. Studies show over 80% of tested drugs retain potency for years beyond the label. But if the pill is discolored, cracked, smells strange, or is liquid that’s cloudy or separated, don’t use it. When in doubt, ask your pharmacist.
What’s the best way to dispose of old pills?
The safest way is to drop them off at a pharmacy or community take-back program. In New Zealand, over 90% of urban areas have these services. If none are nearby, mix pills with coffee grounds or cat litter in a sealed container and throw them in the trash. Never flush unless it’s on the FDA’s flush list-which most meds aren’t.
Do I need to buy expensive software to prevent waste?
No. High-tech systems like Epic or Omnicell help big clinics save 25-30%, but they cost thousands. For homes or small practices, simple methods work just as well: use FIFO (first-in-first-out), check expiration dates weekly, and use color-coded labels. A printed checklist and a $5 fridge thermometer can prevent more waste than most expensive apps.
Why do pharmacies give me so many pills at once?
It’s convenience-and sometimes insurance rules. But you have the right to ask for less. Tell your pharmacist: “I’d like a 30-day supply instead of 90.” Many will split the prescription at no extra cost. This reduces waste, saves money, and helps if your treatment changes.
How can I tell if a medicine has gone bad?
Look for changes: pills that are cracked, discolored, or powdery; liquids that are cloudy, separated, or have particles; creams that smell off or have changed texture. If it looks or smells wrong, don’t use it-even if it’s before the expiration date. Store it properly and dispose of it safely.
Is it safe to share my leftover meds with family?
No. Medications are prescribed based on individual weight, health conditions, allergies, and other factors. What works for you could cause serious harm to someone else-even a close family member. Always dispose of unused meds properly instead of sharing them.
What should I do if my fridge breaks and my insulin gets warm?
If your insulin or other refrigerated medicine was exposed to temperatures above 8°C for more than a few hours, don’t use it. Call your pharmacy or doctor immediately. They can advise if it’s still safe or if you need a replacement. Always keep a thermometer in your fridge and check it weekly to avoid this situation.




swatantra kumar
November 19, 2025 AT 10:32Rebecca Cosenza
November 19, 2025 AT 20:58Sarah Swiatek
November 21, 2025 AT 02:44Pawan Jamwal
November 22, 2025 AT 23:41Dave Wooldridge
November 23, 2025 AT 19:15robert cardy solano
November 24, 2025 AT 19:06rob lafata
November 26, 2025 AT 16:54Lemmy Coco
November 28, 2025 AT 14:51Nick Naylor
November 29, 2025 AT 15:49serge jane
November 30, 2025 AT 10:30Brianna Groleau
December 1, 2025 AT 09:37Bill Camp
December 1, 2025 AT 23:11Matthew McCraney
December 3, 2025 AT 18:37