Lithium-NSAID Risk Calculator
Why This Matters
When you take lithium for bipolar disorder, NSAIDs like ibuprofen can dangerously reduce kidney function, causing lithium to build up. This can lead to severe toxicity or permanent kidney damage.
Immediate Actions
When you're managing bipolar disorder with lithium, even a simple painkiller like ibuprofen can turn dangerous. This isn't a rare edge case - it's a well-documented, life-threatening interaction that happens more often than most doctors and patients realize. Every year, thousands of people on lithium end up in the hospital because they took an over-the-counter NSAID for a headache, back pain, or arthritis flare-up. And in many cases, no one warned them.
Why This Interaction Is So Dangerous
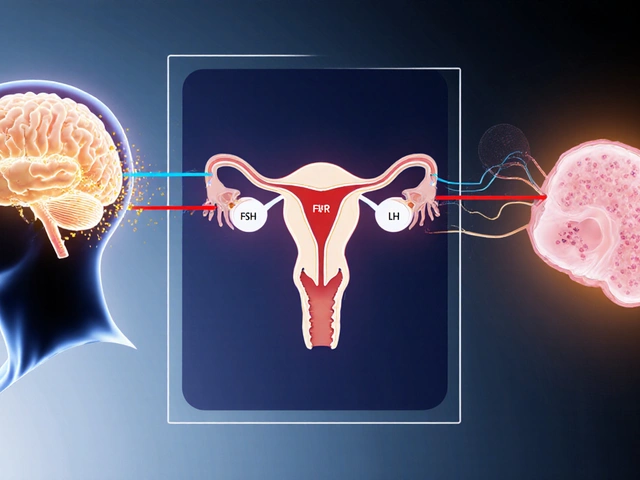
Lithium works by stabilizing mood, but it's a narrow-margin drug. That means the difference between a therapeutic dose and a toxic one is small. Your kidneys are responsible for clearing lithium from your body. When NSAIDs - like ibuprofen, naproxen, or indomethacin - enter the picture, they interfere with how your kidneys work. NSAIDs block enzymes called COX-1 and COX-2, which are needed to make prostaglandins. These prostaglandins help keep blood flowing to your kidneys. When that flow drops, your kidneys slow down. And when they slow down, lithium doesn’t get flushed out. Instead, it builds up. Studies show lithium levels can spike by 20% to 60% within just 48 hours of starting an NSAID. That’s enough to push someone from safe to toxic. The result? Acute lithium toxicity. Symptoms include severe tremors, confusion, slurred speech, muscle weakness, nausea, vomiting, and in worst cases, seizures or coma. But it doesn’t stop there. The damage isn’t always temporary. Repeated exposure can lead to permanent kidney damage - a condition called chronic interstitial nephritis. Some patients end up needing dialysis.Not All NSAIDs Are Created Equal
You might think, "I’ll just pick a milder one." But that’s not enough. The risk varies widely between NSAIDs:- Indomethacin - causes the biggest spike: up to 60% increase in lithium levels
- Piroxicam - increases levels by 25-35%
- Ibuprofen - still risky: 20-30% increase
- Naproxen - similar to ibuprofen, often used long-term for arthritis
- Aspirin - minimal effect at low doses, but still not safe
- Celecoxib - marketed as "kidney-friendly," but still raises lithium by 10-15%
How This Compares to Other Painkillers
What can you take instead? The answer is simpler than you might think.- Acetaminophen (Tylenol) - the safest option. Studies show it doesn’t raise lithium levels at all. But don’t exceed 3,000 mg per day to avoid liver damage.
- Tramadol - sometimes used as a second-line option. It can cause mild lithium increases (10-15%), mostly due to dehydration, so hydration is key.
- Opioids - like oxycodone or hydrocodone, may raise lithium slightly, but mostly through fluid loss. Risk is lower than NSAIDs, but addiction potential makes them a last resort.
- NSAIDs - avoid unless absolutely necessary and under strict monitoring.
Who’s Most at Risk?
This isn’t just a problem for young, healthy people. The highest risk group? Older adults. - People over 65 are 52% more likely to experience lithium toxicity from NSAIDs because kidney function naturally declines with age. - Those with existing kidney disease (eGFR below 60) face exponentially higher risk - even small NSAID doses can trigger acute kidney injury. - Patients seeing multiple doctors - say, a psychiatrist, a primary care provider, and a rheumatologist - are at highest risk. One doctor may not know the other prescribed an NSAID. A 2023 analysis of 478 nephrology clinics found that nearly 40% of all lithium-related kidney injuries were directly tied to NSAID use. And in nearly a third of cases, the NSAID was prescribed by someone who didn’t know the patient was on lithium.
What Doctors Should Do - and Often Don’t
Guidelines are clear. The American Society of Nephrology says: avoid NSAIDs entirely in lithium users. If there’s no alternative, monitor lithium levels twice a week for the first month and check kidney function weekly. But real-world practice? It’s messy. - Only 58% of primary care doctors correctly identify NSAIDs as high-risk for lithium users, according to a national survey. - Only 62% of psychiatrists include NSAID warnings in patient education materials - compared to 99% who warn about diuretics, which carry a similar risk. - Electronic health record alerts exist in 95% of U.S. hospitals, yet they only reduce co-prescribing by 35%. Why? Because they’re often just pop-ups - not hard stops. Some health systems are fixing this. Kaiser Permanente cut lithium-NSAID co-prescribing from 32% to under 12% by making alerts mandatory and requiring provider education. The Veterans Health Administration, however, saw only a small drop - showing how inconsistent implementation can be.What You Should Do If You’re on Lithium
If you take lithium, here’s what you need to know:- Never take an NSAID without talking to your psychiatrist or pharmacist first. Even if it’s "just once."
- Use acetaminophen (Tylenol) as your go-to pain reliever. Stick to 3,000 mg per day max.
- If you’re prescribed an NSAID, ask: "What’s the alternative?" If they say "it’s fine," get a second opinion.
- Hydrate. Drink at least 2.5 to 3 liters of water daily. Especially if you’re taking any new medication.
- Get your lithium levels checked 48-72 hours after starting any new drug. Even if you feel fine.
- Know that the risk lasts. The interaction doesn’t stop when you stop the NSAID. It can take 7-10 days for your kidneys to fully recover.
The Bigger Picture: Why This Keeps Happening
This isn’t just about one bad drug interaction. It’s about how fragmented healthcare is. A patient sees their psychiatrist every three months. But when they hurt their knee, they go to urgent care. The urgent care doctor doesn’t have access to their psychiatric records. They see "bipolar disorder" on the chart but miss the lithium. They write a prescription for ibuprofen. Done. And patients? They don’t know. They think, "I’ve taken Advil for years. Why is this different now?" The economic cost is staggering. In the U.S. alone, lithium-NSAID toxicity leads to $48.7 million in hospital bills every year - $18,450 per hospital stay. And that doesn’t include lost wages, long-term dialysis, or reduced quality of life.
What’s Changing?
There’s hope. The FDA now requires a boxed warning on lithium labels about NSAID interactions. The European Medicines Agency recommends electronic prescribing systems block NSAID prescriptions for lithium users unless a nephrologist signs off. New research is exploring drugs that protect the kidneys during NSAID use - like a prostaglandin analog currently in phase 2 trials. Early results show it cuts lithium level spikes by 87%. But until those treatments are available, the safest strategy remains unchanged: avoid NSAIDs. Use acetaminophen. Stay hydrated. Get regular blood tests. And if your doctor prescribes an NSAID - push back.Frequently Asked Questions
Can I take ibuprofen occasionally if I’m on lithium?
No. Even a single dose of ibuprofen can raise lithium levels by 20-30%, enough to cause toxicity. The risk is highest in the first 72 hours, and symptoms can appear suddenly. There’s no safe "occasional" use. Acetaminophen is the only recommended over-the-counter pain reliever for lithium users.
How long does it take for lithium levels to return to normal after stopping an NSAID?
It can take 7 to 10 days for your kidneys to fully recover and clear lithium normally. Don’t assume you’re safe just because you stopped the NSAID. Continue monitoring your symptoms and get a blood test before resuming your regular lithium dose.
Is aspirin safe to take with lithium?
Low-dose aspirin (81 mg) for heart protection has minimal effect on lithium levels - under 10% increase. But higher doses (like 325 mg or more) act like other NSAIDs and can be dangerous. Always check with your doctor before taking any form of aspirin.
What should I do if I accidentally took an NSAID while on lithium?
Stop taking the NSAID immediately. Drink plenty of water. Contact your psychiatrist or go to an urgent care center to get a lithium blood test within 24-48 hours. Watch for symptoms like tremors, confusion, nausea, or dizziness - these could signal toxicity. Don’t wait.
Are there any new medications for bipolar disorder that don’t interact with NSAIDs?
Yes. Medications like valproate, lamotrigine, and quetiapine are alternatives to lithium and don’t carry the same NSAID interaction risk. However, lithium remains the most effective at preventing suicide in bipolar disorder - reducing risk by 44% compared to 22% with other drugs. Switching isn’t always the answer. The goal is safer pain management while staying on lithium, not abandoning it.





Tanuja Santhanakrishnan
October 30, 2025 AT 13:27Wow, this is such an important post! I’m a pharmacist in India and I see this all the time-patients on lithium grabbing ibuprofen like it’s candy. I always keep a printed handout in my pocket with Tylenol as the go-to and a list of red-flag NSAIDs. Seriously, if you’re on lithium, acetaminophen isn’t just safer-it’s your new best friend. Stay hydrated, get your labs done, and don’t be shy to tell your doctor you’ve read this. Knowledge is power 💪❤️
Raj Modi
October 30, 2025 AT 17:34From a clinical pharmacology standpoint, the mechanism described is not only accurate but also elegantly consistent with renal hemodynamic principles. The inhibition of COX-2-derived prostaglandins, particularly PGE2, leads to afferent arteriolar vasoconstriction, reducing glomerular filtration rate and consequently diminishing lithium clearance via the distal nephron. This is a classic example of pharmacokinetic drug interaction mediated by renal tubular transport dynamics. The 20–60% elevation in serum lithium concentration observed in clinical studies aligns with pharmacokinetic modeling from the 1980s, and the delayed renal recovery window of 7–10 days underscores the need for prolonged monitoring. It is regrettable that this remains under-recognized in primary care settings despite robust evidence.
Stuart Palley
October 31, 2025 AT 11:59Let me tell you something-this is why people die in this country. You think your doctor knows what they’re doing? Nah. They get paid to prescribe. They don’t care if you end up on dialysis. I had a cousin on lithium. Took one Advil for his back. Ended up in the ICU with seizures. No one warned him. No one warned ANYONE. This isn’t a warning-it’s a massacre waiting to happen. And the system? It’s designed to let you fall
Tyler Mofield
November 1, 2025 AT 08:02The data presented is statistically significant and clinically actionable. The American Society of Nephrology’s position statement on lithium-NSAID interactions is unequivocal. The failure of EHR alerts to reduce co-prescribing by more than 35% indicates a systemic failure in clinical decision support architecture. Hard stops are not merely preferable-they are ethically mandatory. The fact that 40% of lithium-related nephrotoxicity cases are attributable to NSAID exposure in the absence of documented psychiatric medication reconciliation constitutes a quality of care crisis. We must implement mandatory e-prescribing barriers and mandatory pharmacist-led reconciliation at point of dispensing.
Lorena Cabal Lopez
November 3, 2025 AT 00:08So… just use Tylenol. That’s it. No drama. No panic. Just don’t take the blue pills.
Karen Werling
November 4, 2025 AT 09:05This made me cry a little. I’ve been on lithium for 12 years. I used to take naproxen for my arthritis like it was nothing. Then my kidneys started acting up. My psychiatrist sat me down and showed me this exact chart. I switched to Tylenol and my labs improved in 3 months. I’m not a doctor but I’ll tell you this-if you’re on lithium, treat your pain meds like your mood meds. They’re both life-or-death. 💛
Cecil Mays
November 5, 2025 AT 12:18THIS IS SO IMPORTANT!!! 🚨 I work in urgent care and I’ve seen 3 patients this month alone come in with lithium toxicity after taking Advil. One guy thought "it’s just a headache"-turned out he was in renal failure. I printed this out and taped it to my desk. Everyone needs to see this. Share it. Tag your doctor. Save a life. ❤️🩺
Sarah Schmidt
November 6, 2025 AT 10:40There’s a deeper metaphysical layer here. The lithium-NSAID interaction is not merely pharmacological-it is symbolic of our fractured relationship with medicine. We treat the body as a machine, yet we ignore the interconnectedness of its systems. We reach for quick fixes-pills for pain, pills for mood-without acknowledging the soul of the patient. The real toxicity isn’t in the drug-it’s in the system that allows ignorance to persist. When we reduce human beings to lab values, we forget that healing requires wisdom, not just data.
Billy Gambino
November 8, 2025 AT 00:42Let’s be honest-the pharmaceutical industry profits from this. If everyone used Tylenol, they’d lose billions. NSAIDs are cheap. They’re everywhere. They’re marketed like candy. Meanwhile, lithium is generic, old, and under-promoted. The fact that celecoxib is still sold as "kidney-friendly" to bipolar patients? That’s not ignorance. That’s negligence dressed in white coats. The FDA warning is too little, too late. We need lawsuits. We need accountability. And we need to stop treating patients like lab rats.
Glenda Walsh
November 8, 2025 AT 22:10Oh my gosh, I’m so glad you posted this!! I just had to tell you-I’m on lithium, and my rheumatologist gave me naproxen last month and I didn’t even realize it was dangerous!! I went to my psychiatrist crying because I had tremors and felt like I was drowning in my own brain!! She checked my levels-4.1!! Normal is 0.6–1.2!! I had to be hospitalized!! Please, if you’re on lithium, PLEASE don’t trust any doctor who says "it’s fine"-they don’t know!! I’m still scared!!
STEVEN SHELLEY
November 8, 2025 AT 22:13THIS IS A GOVERNMENT COVERUP. NSAIDs are NOT the problem. The real danger is lithium itself. The FDA knows this. The VA knows this. They’re pushing this narrative to keep you dependent on a toxic drug that was developed during the cold war. Tylenol? That’s a Monsanto product. They own the labs. They own your doctors. Your kidneys are fine. It’s your mind they’re poisoning. Don’t trust anyone. Get off lithium. Go natural. Drink lemon water. Meditate. The system wants you sick.
Emil Tompkins
November 9, 2025 AT 21:00So let me get this straight… you’re telling me I can’t take ibuprofen for my back pain but I can take tramadol? Which is literally a synthetic opioid? That’s not safer-that’s just swapping one nightmare for another. And acetaminophen causes liver failure? So what am I supposed to do? Lie on the floor and scream? This isn’t medicine-it’s a trap. And now I’m supposed to drink 3 liters of water every day? I’m not a camel. I’m a person with bipolar disorder and a bad back. Who designed this system? A robot?
Kevin Stone
November 10, 2025 AT 14:08Interesting post. But you’re ignoring the fact that many patients have comorbid conditions. Arthritis is chronic. Acetaminophen doesn’t work for everyone. And tramadol has its own risks-seizures, serotonin syndrome. The real issue isn’t the interaction-it’s the lack of alternatives. We need better mood stabilizers that don’t require such extreme pain management restrictions. Until then, we’re just managing a broken system.
Natalie Eippert
November 11, 2025 AT 19:20As an American citizen I find this deeply concerning. Our healthcare system has become a joke. We have people dying because doctors don’t communicate and patients don’t read labels. This is why we need stronger borders-not just for people but for dangerous prescriptions. No more mixing foreign drugs with American patients. We need a national standard. No NSAIDs for lithium users. Period. And if you can’t follow that rule, you shouldn’t be prescribing.
kendall miles
November 13, 2025 AT 16:47There’s a reason this isn’t common knowledge. The lithium industry is tied to the psychiatric-industrial complex. In New Zealand, we’ve had fewer cases because we use different protocols. But here? They’re pushing lithium because it’s cheap. They don’t care about your kidneys. They care about your compliance. And your compliance means profit. This post is a wake-up call-but only if you’re brave enough to question everything.