Pediatric Antihistamine Dosing Calculator
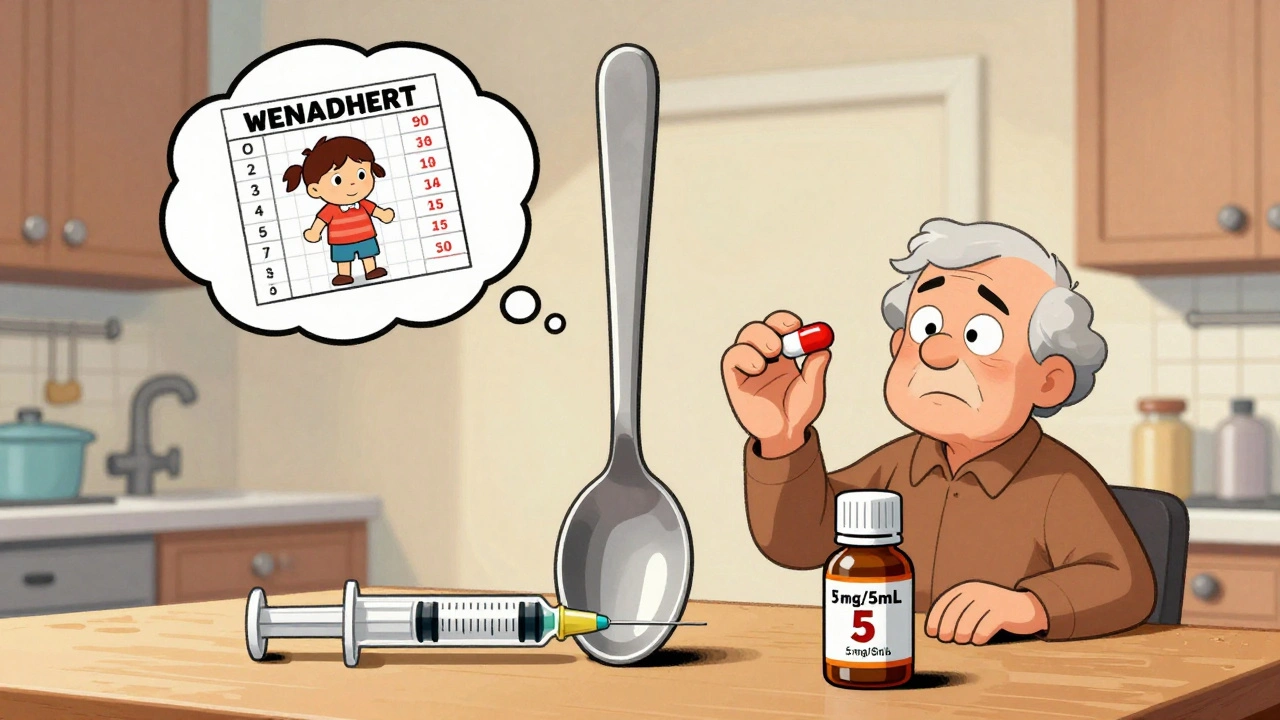
Every year, thousands of children end up in emergency rooms because of a simple mistake: the wrong dose of an antihistamine. It’s not because parents are careless. It’s because the system is confusing. Liquid bottles look similar. Charts use different numbers. Kitchen spoons aren’t accurate. And when your child is sneezing or itchy, you just want to make it stop-fast.
Why Pediatric Antihistamine Dosing Is So Risky
The most common antihistamines used for kids are diphenhydramine (Benadryl), loratadine (Claritin), and cetirizine (Zyrtec). But they’re not created equal. First-generation drugs like Benadryl cross the blood-brain barrier easily. That’s why they make adults drowsy-and why they can cause dangerous side effects in children: agitation, rapid heartbeat, seizures, even breathing problems. According to the American Association of Poison Control Centers, over 21,000 children under 6 were exposed to antihistamines in 2022. Nearly 80% of emergency visits for these cases involved kids under 6. And the biggest culprit? Diphenhydramine. Even though second-generation antihistamines like Claritin and Zyrtec are safer and just as effective for allergies, many parents still reach for Benadryl because it’s cheaper, familiar, or they think it works faster. Here’s the truth: Benadryl isn’t meant for daily use in young kids. The FDA and the American Academy of Pediatrics both warn against using it for colds or routine allergies in children under 2. Yet, 67% of pediatricians say they still see parents giving it for runny noses and coughs. That’s not just ineffective-it’s risky.The Measurement Problem: Kitchen Spoons Are Not Safe
One of the most dangerous myths is that a teaspoon is a teaspoon. It’s not. A standard kitchen teaspoon can hold anywhere from 2.5 to 7.5 milliliters. That’s a 300% difference. A child who needs 5 mL of Zyrtec could get 15 mL if you use a big spoon-and that’s enough to send them to the hospital. The FDA has required all pediatric liquid medications to come with a dosing device since 2011. That device should be an oral syringe or a dosing cup marked in milliliters only. But a 2018 study in Pediatrics found that 42% of parents still use kitchen spoons, shot glasses, or even droppers not meant for medicine. Here’s what you need to know:- 5 mL = 1 teaspoon (but never use a kitchen spoon)
- 15 mL = 1 tablespoon
- Always use the syringe that came with the bottle
- Never use a syringe from a different medicine
Dosing by Weight, Not Age
Age-based dosing charts are outdated and dangerous. A 2-year-old weighing 20 pounds needs a different dose than a 2-year-old weighing 30 pounds. The correct dose is based on weight, not birthday. Here’s what the most reliable pediatric guidelines recommend as of 2023:| Weight | Diphenhydramine (Benadryl) | Loratadine (Claritin) | Cetirizine (Zyrtec) |
|---|---|---|---|
| 20-24 lbs | 3.75 mL (12.5 mg/5mL liquid) | 2.5 mL (5 mg/5mL liquid) | 2.5 mL (5 mg/5mL liquid) |
| 25-37 lbs | 5 mL (12.5 mg/5mL liquid) | 5 mL (5 mg/5mL liquid) | 5 mL (5 mg/5mL liquid) |
| 38-49 lbs | 7.5 mL (12.5 mg/5mL liquid) | 7.5 mL (5 mg/5mL liquid) | 7.5 mL (5 mg/5mL liquid) |
| 50+ lbs | 10 mL (12.5 mg/5mL liquid) | 10 mL (5 mg/5mL liquid) | 10 mL (5 mg/5mL liquid) |
Notice something? The liquid concentrations differ. Benadryl is 12.5 mg per 5 mL. Claritin and Zyrtec are both 5 mg per 5 mL. That means if you accidentally use the same syringe for both, you’re giving your child double the dose of loratadine or cetirizine. That’s why you need a separate syringe for each medication.
And don’t assume chewables are safer. The FDA’s MAUDE database reports that 12% of pediatric medication errors involve choking on tablets. For kids under 4, liquid or dissolvable forms are always preferred.
Second-Generation Antihistamines Are Safer-And Simpler
Loratadine and cetirizine are second-generation antihistamines. They don’t cross the blood-brain barrier as easily, so they cause less drowsiness and have a much wider safety margin. The therapeutic index (the gap between a safe dose and a toxic one) for diphenhydramine is about 2:1. For cetirizine, it’s 10:1. That means you’d need to give five times the right dose of Zyrtec to reach a dangerous level-compared to just twice the dose with Benadryl. Plus, they’re once-daily. Benadryl needs to be given every 4-6 hours. That’s up to four doses a day. More chances for mistakes. More chances for confusion. More chances for a tired parent to give a second dose thinking the first didn’t work. A 2023 study in the Journal of the American Pharmacists Association found that pharmacists catch 19% of pediatric antihistamine prescriptions before they’re filled-almost always because someone tried to use an adult tablet or misread the concentration. That’s not a failure of parents. It’s a failure of the system.What You Can Do Right Now
You don’t need to be a doctor to keep your child safe. Here’s your action plan:- Use only liquid formulations with an oral syringe. Never use a kitchen spoon.
- Check the concentration on the bottle. Is it 12.5 mg/5 mL? Or 5 mg/5 mL? Write it down.
- Dose by weight, not age. Use a pediatric scale if you can. If not, estimate based on growth charts.
- Use the same syringe for the same medicine. Never reuse a syringe from another drug.
- Ask your pharmacist to show you how to measure it. Do it out loud. Say: “I’m giving 3.75 mL for 22 pounds.” Then do it again.
- Store all medicines out of reach. Grandparents, babysitters, older siblings-they all need to know the rules.
One parent on Reddit shared that she started using the MedsHelper app. It shows a visual syringe, asks her to confirm the child’s weight, and even plays a voice recording of the dose. She said it cut her anxiety in half. That’s not magic. That’s good design.

When to Call Poison Control
If you think your child got too much antihistamine, don’t wait. Don’t Google. Don’t ask Facebook. Call Poison Control immediately: 1-800-222-1222. They’re available 24/7, free, and trained to walk you through what to do. Signs of overdose include:- Extreme drowsiness or inability to wake up
- Fast or irregular heartbeat
- Flushed skin or dry mouth
- Difficulty breathing
- Seizures or uncontrolled movements
Even if your child seems fine, call anyway. Some effects take hours to show up. And remember: 31% of all antihistamine calls to Poison Control are from parents who are unsure if they gave the right dose. You’re not alone. And help is just one call away.
The Bigger Picture: Why This Keeps Happening
This isn’t just about parents making mistakes. It’s about outdated labels, inconsistent charts, and a lack of standardized education. Some hospitals use one weight chart. Others use another. Some recommend 2.5 mg for kids 2-5 years. Others say 5 mg. That’s not a small difference-it’s life-changing. The good news? Change is coming. The FDA is testing QR codes on medicine bottles that link to video instructions. Pilot programs at Boston Children’s Hospital showed a 53% drop in dosing errors. Children’s hospitals are now using electronic health records that auto-calculate doses based on weight and flag unsafe prescriptions. But until every bottle has clear, consistent instructions-and every caregiver knows how to use a syringe-your vigilance is the most powerful tool you have.Antihistamines are not harmless. They’re powerful drugs. And for kids, the margin for error is razor-thin. You don’t need to be perfect. You just need to be careful. Use the right tool. Dose by weight. Ask questions. And when in doubt-call.
Can I give my 1-year-old Benadryl for allergies?
No. The FDA and American Academy of Pediatrics strongly advise against using first-generation antihistamines like diphenhydramine (Benadryl) in children under 2 years old. The risk of serious side effects-including seizures, breathing problems, and extreme drowsiness-is too high. For allergies in babies, consult your pediatrician. Second-generation antihistamines like cetirizine or loratadine may be approved for use starting at age 6 months, but only under medical supervision.
Is it safe to use a kitchen teaspoon if I don’t have a syringe?
No. A kitchen teaspoon can hold anywhere from 2.5 to 7.5 milliliters, which means you could be giving your child up to three times the intended dose. This is one of the most common causes of antihistamine overdoses in children. Always use the oral syringe or dosing cup that came with the medicine. If you lost it, call your pharmacy-they’ll give you a new one for free.
What’s the difference between Children’s Zyrtec and regular Zyrtec?
Children’s Zyrtec is a liquid formulation with a concentration of 5 mg per 5 mL. Regular Zyrtec is a 10 mg tablet. Giving a child a whole adult tablet is dangerous and can lead to overdose. Always check the label. If it says “10 mg,” it’s for adults only. For children, use the liquid version with the dosing syringe.
Can I give my child Claritin and Benadryl together?
Never combine antihistamines unless your pediatrician specifically tells you to. Both Claritin and Benadryl work the same way. Giving them together increases the risk of side effects like drowsiness, dry mouth, and rapid heartbeat. If one isn’t working, talk to your doctor before switching or adding another medication.
How do I know if I gave my child the right dose?
First, weigh your child. Then, check the label on the medicine bottle for the concentration (mg per mL). Use the dosing syringe that came with the bottle. Measure the exact number of milliliters based on weight. If you’re unsure, call your pharmacist. They’ll walk you through it. And remember: if your child seems unusually sleepy, agitated, or has trouble breathing, call Poison Control immediately.
Are chewable antihistamines safe for toddlers?
Chewable tablets are not recommended for children under 4 years old because of choking risk. The FDA reports that 12% of pediatric medication errors involve choking on tablets. For young children, always use liquid formulations with a dosing syringe. If your child is older than 4 and can safely chew and swallow, chewables can be an option-but still use the correct weight-based dose.






Himmat Singh
December 12, 2025 AT 22:04The premise of this article is fundamentally flawed. Antihistamines are not 'dangerous drugs'-they're tools. The real issue is parental ignorance, not systemic failure. If you can't read a label or measure a teaspoon, maybe you shouldn't be medicating your child at all. Blaming the system is convenient, but it shifts responsibility away from the people who actually hold the syringe. This isn't a public health crisis-it's a parenting crisis.
Donna Hammond
December 14, 2025 AT 03:42I’m a pediatric nurse, and I see this every single week. One parent used a kitchen spoon because ‘it was all they had.’ Their 18-month-old ended up in ICU with tachycardia and agitation. This isn’t theoretical-it’s real life. Please, please, please: use the syringe. Write the dose on your hand if you have to. Keep meds locked up. And if you’re unsure? Call your pharmacist. They don’t judge. They just want your kid to be safe. You’re not alone in this. 💪
Richard Ayres
December 14, 2025 AT 18:29This is one of the most well-researched and practical pieces I’ve read on pediatric medication safety. The emphasis on weight-based dosing over age-based charts is critical. Many clinicians still default to age, which is outdated and dangerous. The data on concentration differences between Benadryl and Zyrtec is especially important-most caregivers don’t realize that using the same syringe for both can double the dose of the second-gen antihistamine. The FDA’s QR code pilot is promising, but until it’s universal, education and clear labeling remain our best tools. Thank you for writing this.
Jennifer Taylor
December 15, 2025 AT 10:46Okay but have you seen what’s REALLY going on? 😱 Big Pharma doesn’t want you to know this-Benadryl is being pushed because it’s cheap and they make billions off it. The FDA? They’re in bed with the drug companies. They only ‘approved’ the syringes because of PR pressure after a few kids died. The real reason Zyrtec and Claritin aren’t everywhere? They’re patented and expensive. And don’t get me started on how the government hides the truth about antihistamine side effects… I’ve got screenshots. DM me. 🚨
Shelby Ume
December 16, 2025 AT 07:21As a mom of three and a former pharmacy tech, I want to say: this article saved my life. I used to use kitchen spoons. I thought 'a teaspoon is a teaspoon.' I didn’t know the concentration difference between Benadryl and Zyrtec. I didn’t know you had to dose by weight. I thought I was doing fine. Then my youngest had a reaction. Now I use the MedsHelper app too. I keep the syringes in a labeled drawer. I show my mom and babysitter how to measure. It’s not about being perfect. It’s about being intentional. You can do this. 💕
Jade Hovet
December 16, 2025 AT 09:34OMG YES!! I just started using the syringe and now I feel like a superhero 😍 I used to guess with spoons and now I’m like ‘ok 5.5 mL for 32 lbs’ and I even take a pic of the bottle so I don’t forget. My toddler doesn’t even cry anymore bc I’m calm now. Also-got a free syringe from the pharmacy last week!! They gave me a sticker too 🤗 #ParentingWin
nithin Kuntumadugu
December 17, 2025 AT 05:27Lmao this is so basic. You're all overreacting. Kids have been taking Benadryl since the 50s. My cousin took it at 1 and turned out fine. You think a 'dosing syringe' is gonna fix a generation of lazy parents? 😴 The real problem? Too many apps, too much tech, too many rules. Just give 'em the damn liquid. If they sleep too much, they sleep too much. Kids are tougher than you think. Stop panicking. 🤷♂️
John Fred
December 18, 2025 AT 19:28As a clinical pharmacist, I’ll add one thing: the 12.5 mg/mL vs 5 mg/mL concentration trap is the #1 error we catch. Parents think 'it’s all the same blue liquid' and grab whichever syringe is handy. We’ve had cases where a kid got 20 mL of Benadryl thinking it was Zyrtec-because both are blue. Always check the mg/mL. Always. And if you’re using a syringe from another med? Stop. Right now. We’re not trying to scare you-we’re trying to save you from a 72-hour hospital stay. 🙏
Harriet Wollaston
December 20, 2025 AT 00:37I’m from Nigeria and we don’t even have syringes in some villages. We use the cap from the bottle or a medicine spoon from the market. This article made me realize how lucky I am to live where I do. But it also made me want to share this with my family back home. Maybe I can translate it. Because safety shouldn’t depend on where you’re born. Thank you for writing this with so much care.