If a plant could lower blood pressure fast, why did doctors abandon it? American hellebore (Veratrum viride) did exactly that a century ago-and sent people crashing with slow heart rates, vomiting, and dangerous drops in blood pressure. Today, it sometimes pops up online as a “natural supplement” for better health. Here’s the straight talk: this is not a safe dietary supplement. I’ll explain what it is, the claims vs actual evidence, the real risks, how poisonings happen, and what to use instead that’s backed by better data. If you found this page because you were considering a American Hellebore supplement, please read this before you buy or take anything.
- TL;DR: American hellebore is a poisonous plant, not a safe supplement. Modern regulators do not recognize it as safe for self-care.
- Claims (blood pressure, pain, immunity) are not backed by solid human evidence. Case reports of poisoning are well-documented.
- Main risks: severe nausea/vomiting, bradycardia, hypotension, confusion, and fetal harm. Cooking or drying does not make it safe.
- Online products can be mislabeled. Learn how to spot red flags and avoid dangerous botanicals.
- Safer alternatives exist for every “benefit” people chase hellebore for-like magnesium or beetroot for blood pressure, ginger for nausea, and simple lifestyle wins.
What American hellebore actually is-and why it’s not a safe supplement
American hellebore (Veratrum viride) is a tall, leafy plant native to North America. It also goes by false hellebore, Indian poke, and green hellebore. It’s not the same as the ornamental Christmas rose (Helleborus species). Different plant families, different toxins-both risky in their own ways.
The danger comes from steroidal alkaloids (like jervine-family compounds) that act on sodium channels and the vagus nerve. That combo can slow the heart, drop blood pressure, trigger vomiting, and cause neurological symptoms. Historical medical texts from the late 1800s and early 1900s describe using Veratrum viride tinctures to lower high blood pressure or calm rapid pulse, but side effects were so severe and unpredictable that it fell out of favor as safer drugs emerged. It was once included in early editions of the U.S. Pharmacopeia; it’s no longer there and has not been an approved modern medicine for decades.
Where do regulators stand today? In the United States, the Food and Drug Administration does not approve Veratrum viride for any medical use. Poison control centers regularly warn against ingesting false hellebore. The NIH Office of Dietary Supplements does not provide a monograph endorsing its use. In Europe, pharmacopoeias and the European Medicines Agency focus on safety concerns with Veratrum species rather than any therapeutic role. In New Zealand and Australia, food and medicines regulators take a conservative stance on toxic botanicals; a product sold with health claims that includes Veratrum would likely be treated as a medicine and face serious safety scrutiny.
Bottom line: this plant was pulled out of modern practice for a reason. The “natural” label doesn’t erase risk. With American hellebore, risk is the headline.
Claims vs evidence: what history and science actually show
You might see online shops or forums claim benefits like “blood pressure support,” “pain relief,” “calming,” “immune boost,” or “detox.” Here’s how those claims stack against what we know.
| Health claim | Best available evidence | Risk profile |
|---|---|---|
| Lower blood pressure / slow rapid heart rate | Historical use documented; modern randomized trials are lacking. Older medical literature notes frequent severe side effects. No current guideline recommends it. | High: bradycardia, hypotension, syncope. Dangerous with heart meds or dehydration. |
| Pain relief or calming | No quality human trials. Any perceived effects may reflect toxicity (sedation, malaise), not therapeutic benefit. | High: nausea, vomiting, confusion; risk outweighs unproven benefits. |
| Immunity / detox / weight loss | No credible human evidence. These are marketing claims without scientific backing. | High: systemic toxicity with no proven upside. |
| Topical use for aches | Skin absorption of Veratrum alkaloids can occur. Case reports show systemic poisoning even with non-oral exposure. | High: not safe, even externally. |
Real-world incidents tell the story. U.S. poison control data and CDC field reports describe clusters of false hellebore poisoning after people foraged it by mistake, thinking it was edible wild leek. Symptoms commonly start with intense nausea and vomiting, then dizziness, slow heart rate, and low blood pressure. Emergency care is often needed. In veterinary and agricultural literature, related Veratrum species caused severe birth defects in livestock; a compound from a western species (cyclopamine) famously disrupted fetal development in sheep-a stark reminder that these alkaloids are biologically powerful in the wrong ways.
Traditional Chinese medicine texts also warn about Veratrum (often called Li Lu) as highly toxic and incompatible with many common herbs. That’s not an endorsement; it’s another caution flag that crosses cultures.
What about “microdosing”? With plants like Veratrum, the margin between “dose” and “poison” is thin and variable depending on the part of the plant, season, and preparation. Home kitchen tinctures or powders make that line even fuzzier. This is not something to experiment with.
Risks, side effects, and how poisonings happen (and what to do)
Here’s what typically shows up in case reports and poison center data:
- Onset: 30 minutes to a few hours after ingestion (or sooner with tinctures). Topical exposures can also cause systemic effects.
- Common symptoms: burning mouth, intense nausea, repeated vomiting, diarrhea, dizziness, tingling, sweating.
- Cardiovascular: bradycardia (slow pulse), hypotension (low blood pressure), rhythm changes, fainting.
- Neurological: weakness, confusion, blurred vision, rarely seizures.
- Pregnancy: teratogenic potential is a serious concern; related alkaloids have caused fetal defects in animals. Avoid entirely.
Who is at higher risk of severe outcomes?
- Anyone on heart or blood pressure medications (beta-blockers, calcium channel blockers, ACE inhibitors), digoxin, or diuretics.
- People with heart rhythm issues, low blood pressure, electrolyte problems, or dehydration.
- Children, older adults, and pregnant people.
How poisonings happen:
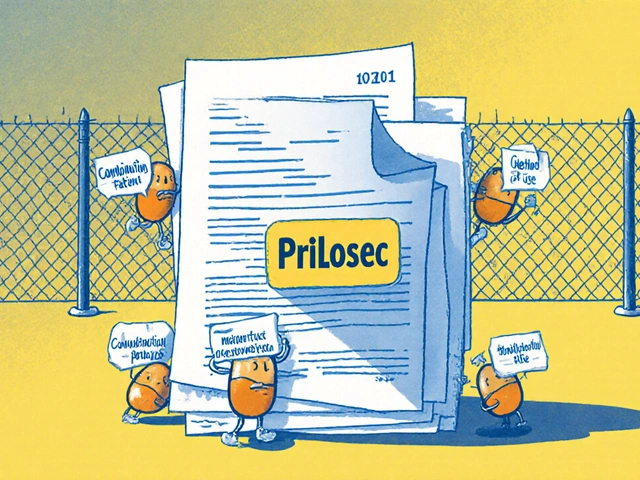
- Mislabeled “herbal supplements” bought online, often from unverified sellers, using botanical names loosely or blending multiple species.
- Home-made tinctures or teas from foraged plants misidentified as wild leek, ramps, or skunk cabbage.
- Topical liniments made from Veratrum species, applied over large areas or broken skin.
Immediate actions if exposure happens:
- Stop using the product and do not try to “flush it out” with alcohol or other herbs.
- If the person has severe vomiting, dizziness, fainting, chest discomfort, or a very slow heart rate, seek emergency care immediately.
- Contact your local poisons hotline or emergency department for advice even if symptoms seem mild; effects can progress.
- Keep the product container or plant sample-health professionals may need it to identify the toxin.
- Report the incident: In the U.S., use FDA MedWatch for dietary supplement adverse events; in New Zealand, report to the Centre for Adverse Reactions Monitoring (CARM). This helps regulators act.
Red flags on product labels:
- Botanical names that include “Veratrum,” “false hellebore,” or vague blends without Latin binomials.
- Promised effects like “instant blood pressure fix,” “detox,” “cancer fighter,” or “replace your meds.”
- No third-party testing seals (USP, NSF, Informed Choice) and no batch lot numbers.
- Imported powders with no country of origin, no manufacturer, or no way to contact the seller.

Safer alternatives that actually support better health
If you were curious about American hellebore, you were probably chasing one of a few goals: lower blood pressure, calm the nervous system, ease nausea or pain, or “detox.” You can get those goals without flirting with a poison.
For blood pressure:
- Beetroot juice or nitrate-rich veggies: Controlled studies show dietary nitrate can modestly lower systolic BP. Aim for regular servings of beetroot, rocket, or spinach. If you consider a nitrate supplement, talk with your clinician first if you’re on BP meds.
- Magnesium glycinate or citrate: Often 200-400 mg elemental magnesium daily supports small BP reductions and better sleep. Avoid high doses if you have kidney disease.
- Lifestyle power trio: 30 minutes of brisk walking most days, cutting sodium to under 2,000 mg/day, and getting 7-8 hours of sleep can beat many pills for impact when done consistently.
For nausea:
- Ginger extract or tea: Multiple randomized trials support ginger (often 1 gram/day in divided doses) for mild nausea, including motion sickness and pregnancy (check with your clinician if pregnant).
- Acupressure bands (P6 point): Low-risk and helpful for many people.
For stress and sleep:
- Magnesium (as above) and L-theanine (100-200 mg): Evidence supports small but meaningful calming effects.
- Light, routine, and screens: Morning daylight plus a fixed bedtime often beats any supplement within two weeks.
For aches:
- Topical NSAIDs (like diclofenac gels) have solid evidence for localized pain and low systemic risk when used as directed.
- Heat for muscle tightness; ice for acute flare-ups. Simple, effective, and safe.
About “detox”:
- Your liver and kidneys already do this job. Support them by skipping binge drinking, staying hydrated, eating fiber (veg, legumes), and sleeping well.
- If you suspect a specific exposure (e.g., heavy metals), skip DIY protocols and get proper testing and care.
How to vet any herbal product before it reaches your cart:
- Demand a Latin binomial, plant part, standardization, and batch number on the label.
- Look for third-party testing (USP, NSF, Informed Choice). No seal? That’s a pass for me.
- Avoid proprietary blends that hide how much of each ingredient you’re getting.
- Search the ingredient on your national poisons centre or regulator site. If a plant is known to be toxic, don’t negotiate with it.
- Check interactions. The NIH Office of Dietary Supplements and your pharmacist are good starting points.
A quick decision guide:
- If your goal is lower BP within weeks: try diet changes + magnesium + walking. Recheck readings with a validated cuff. If you’re already on meds, coordinate any supplement with your clinician to avoid hypotension.
- If your goal is calm sleep: set a 30-minute pre-bed wind-down, limit caffeine after midday, and consider magnesium or L-theanine.
- If your goal is nausea relief: ginger first; if persistent, look for the cause (migraine, reflux, meds) rather than piling on herbs.
- If your goal is “detox”: define the problem you want to solve. “Feel lighter” is usually sleep + fiber + hydration, not a plant extract.
Mini‑FAQ
Is American hellebore the same as the Christmas rose hellebore I see in gardens? No. American hellebore is Veratrum viride; the garden plants are Helleborus species. Both can be toxic, but they’re different plants.
Does cooking or drying make American hellebore safe? No. Heat and drying don’t reliably neutralize the alkaloids. People have gotten very sick from cooked plants misidentified in the wild.
What about homeopathic Veratrum viride? High-dilution homeopathic products typically contain no measurable alkaloids and are not the same as herbal extracts. They’re generally considered low risk from a toxicity standpoint, but they also don’t provide the pharmacologic effects people expect from herbs.
Could tiny “microdoses” of the herb be safe? Dosing is unpredictable. Alkaloid levels vary by plant part and season. The safety margin is thin. This is not a candidate for self-experimentation.
Is topical use okay if I don’t swallow it? No. Alkaloids can absorb through skin, especially with oils, heat, or broken skin. Poisonings have occurred after topical use.
Can pets get poisoned? Yes. Keep pets away from any Veratrum species and any product containing them.
How do I report a bad reaction? In the U.S., use FDA MedWatch. In New Zealand, report to CARM. Your local poisons centre can guide you.
Next steps and troubleshooting
If you were about to buy American hellebore: Don’t. Choose one safe alternative that matches your goal and give it 2-4 weeks while you track results (blood pressure, sleep hours, or symptom notes). One change at a time beats a handful of guesswork.
If you already bought a product labeled Veratrum/false hellebore: Do not use it. Dispose of it safely (sealed, out of reach of kids and pets). If you’ve taken any and feel unwell-nausea, dizziness, slow pulse-seek medical help and contact your poisons hotline.
If you forage: Learn plant ID from local experts and cross-check with a trusted field guide. False hellebore’s pleated leaves can fool people into thinking it’s edible wild leek, but it lacks the onion smell and has different leaf structure. When in doubt, leave it.
If you’re a clinician: Suspect Veratrum with GI distress plus bradycardia/hypotension after foraging or herbal use. Supportive care, fluids, atropine for symptomatic bradycardia as appropriate, and monitor electrolytes. Report to public health if multiple cases suggest a cluster.
If you’re a retailer: If any supplier pitches Veratrum species for ingestion or topical use, decline the product and alert your regulator. This is not a reputational risk you want.
Credibility check-who says it’s risky? The U.S. FDA does not approve Veratrum as safe or effective; the NIH’s Office of Dietary Supplements does not support its use; the American Association of Poison Control Centers and CDC have documented poisonings; European and Australasian regulators treat Veratrum as a dangerous plant, not a health aid. That’s a wide, consistent safety signal.
One last sanity tip: if an herb was once a hospital drug but got abandoned for safety, don’t reintroduce it in your kitchen. You deserve options that are both effective and safe.





Renee Zalusky
September 18, 2025 AT 13:53okay but like… why does this stuff keep popping up online? i saw a tiktok ad for ‘ancient american heart remedy’ and thought it was a joke. turns out it’s real. someone’s making bank off people who think ‘natural’ = safe. my grandma took foxglove for her heart in the 70s and ended up in the er. same energy. 🤦♀️
Scott Mcdonald
September 18, 2025 AT 14:33bro i just bought a bottle of this off amazon last week lol. thought it was some kind of ‘herbal coffee’ for energy. now i’m kinda scared. should i flush it or just leave it in the cabinet and pretend it never happened?
Victoria Bronfman
September 19, 2025 AT 15:49OMG I’M SO GLAD YOU WROTE THIS. 🙌 I was literally about to order some ‘Veratrum Viride Tincture’ because the label said ‘ancient Native American wisdom’ and had a sunset on it. 🌅💀 Now I’m deleting my cart and buying beetroot powder instead. #DontBeAFool #NaturalIsntAlwaysNice
Gregg Deboben
September 21, 2025 AT 11:47THIS IS WHY AMERICA IS FALLING APART. People think they can replace real medicine with some dirt from the woods. We had doctors who knew what they were doing, and now we got TikTok healers selling poison like it’s kombucha. 🇺🇸 STOP THIS. CALL THE FDA NOW. THIS ISN’T A ‘CHOICE’-IT’S A PUBLIC HEALTH DISASTER.
Christopher John Schell
September 22, 2025 AT 23:46you’re doing the world a favor by writing this. 🙏 i used to think ‘if it’s natural, it’s harmless’ - until my cousin ended up in the hospital after trying ‘wild garlic’ that turned out to be false hellebore. don’t gamble with your heart. the alternatives you listed? those are real. try one for 30 days. your body will thank you. 💪
Felix Alarcón
September 23, 2025 AT 14:59hey, i’m from mexico and we have a similar plant called ‘cabeza de negro’ - super toxic, used in folk remedies but always with extreme caution. elders used to say: ‘if it makes you vomit and your heart skip, it’s not medicine, it’s a warning.’ your post reminded me of that. thanks for keeping it real. 🙏
Lori Rivera
September 25, 2025 AT 03:39While the article is thorough and well-referenced, I would appreciate a more explicit discussion on the regulatory loopholes that allow such products to be sold as ‘dietary supplements’ despite lacking GRAS status. The FDA’s enforcement capacity is limited, and this represents a systemic failure in consumer protection policy.
Leif Totusek
September 25, 2025 AT 11:20Thank you for the clear, science-based breakdown. I’ve shared this with my elderly parents who were considering trying ‘herbal BP support.’ They now understand the risks. I wish more health content was this responsible.
KAVYA VIJAYAN
September 25, 2025 AT 20:32From a pharmacognosy perspective, the steroidal alkaloids in Veratrum viride-particularly jervine and cyclopamine-are fascinating in their mechanism of action. They act as potent inhibitors of the Hedgehog signaling pathway, which explains both the teratogenic effects and the hypotensive potential. But here’s the kicker: the therapeutic index is essentially nonexistent. Unlike digitalis, which has a narrow but manageable window, Veratrum’s variability in alkaloid concentration across plant parts, seasons, and soil conditions makes dosing a gamble with lethal stakes. The fact that it was ever in the U.S. Pharmacopeia is a relic of pre-pharmacokinetic medicine. Today, we have precision tools: ACE inhibitors, beta-blockers, even SGLT2 inhibitors. Why risk a pre-industrial toxin when we have molecules engineered for safety profiles? The real tragedy isn’t the plant-it’s the misinformation economy that repackages ancient danger as ‘biohacking.’
Jarid Drake
September 27, 2025 AT 06:24just read this after my friend sent me the link. i almost bought some ‘heart tonic’ off Etsy last month. ugh. thanks for the scare. going to go drink some beet juice now 😅
Tariq Riaz
September 27, 2025 AT 19:31Interesting how the article conflates traditional use with modern safety. Many cultures used toxic plants medicinally-belladonna, aconite, even opium. The absence of evidence isn’t evidence of absence. But the burden of proof lies with the user, not the regulator. Still, the documented poisoning cases are too numerous to ignore. A nuanced view: the plant is dangerous, yes-but the real issue is the lack of education, not the plant itself.
Roderick MacDonald
September 29, 2025 AT 13:52Look, I get it-people are desperate. Chronic high BP, anxiety, sleep issues… it’s exhausting. And when Big Pharma feels expensive or impersonal, it’s tempting to turn to something ‘natural’ that feels like it’s been around forever. But here’s the truth: nature doesn’t care if you’re trying to feel better. It doesn’t have your best interests at heart. The alternatives you listed? They’re not just ‘safer’-they’re actually *better*. Beetroot, magnesium, ginger, walking-they work. They’re proven. And they don’t put you in the ER. So if you’re reading this and thinking ‘maybe just a tiny bit’-stop. Choose the path that doesn’t require a poison control call. You’ve got this. 💙