Getting the right dose of liquid medicine isn’t just about following instructions-it’s about staying safe. Every year, over 1.3 million people in the U.S. are injured because someone took the wrong amount of liquid medication. Most of these errors happen because people misread the label. You’re not alone if you’ve stared at a bottle and wondered: Is that 0.5 mL or 5 mL? Should I use a spoon? What does 120 mg/5 mL even mean?
What You’ll See on the Label
Every liquid prescription label has three key pieces of information you need to read carefully: concentration, dosage amount, and total volume. These aren’t just words-they’re instructions for your safety.
The concentration tells you how much medicine is in each milliliter. It’s written like this: 120 mg/5 mL. That means every 5 milliliters of liquid contains 120 milligrams of the drug. If your doctor prescribed 60 mg, you don’t take half the bottle-you take half of 5 mL, which is 2.5 mL. Confusing the concentration with the dose is one of the most common mistakes. A parent once told me they gave their child the full 5 mL because they thought the 120 mg was the total dose, not the amount per 5 mL. That’s how overdoses happen.
The dosage amount is what you’re supposed to take at one time. It’s usually written clearly: Take 5 mL every 6 hours. Never assume. If it says Take 2.5 mL, don’t round up to 3 mL because that’s easier. Small differences matter, especially for kids and babies.
The total volume is the size of the bottle-like 100 mL or 150 mL. This tells you how long the prescription will last, but it’s not the dose. I’ve seen people think they need to take the whole bottle because it says 150 mL on the side. That’s dangerous. Always ignore the total volume when figuring out how much to take.
Why Milliliters (mL) Are the Only Unit You Should Trust
Look closely. The label should only use milliliters (mL)-never teaspoons, tablespoons, or drops. That’s not a suggestion. It’s a rule. The FDA and the National Council for Prescription Drug Programs (NCPDP) banned non-metric units on prescriptions in 2016 because household spoons are wildly unreliable.
A teaspoon from your kitchen? It could hold anywhere from 2.5 mL to 7.5 mL. A tablespoon? It might be 5 mL or 20 mL. That’s a 300% difference. A 2016 study in the Journal of Pediatrics found parents using spoons were twice as likely to give the wrong dose. For a baby, that could mean the difference between a safe dose and a hospital visit.
Even if the label says “1 tsp,” don’t use a spoon. That’s a legacy error. By 2020, 92% of major pharmacy chains like CVS and Walgreens stopped using teaspoons on labels. If you see one, ask the pharmacist to rewrite it in mL. They’re required to do it.
How to Read Numbers Correctly
Numbers on labels follow strict rules to prevent deadly mistakes.
- Always use a leading zero: Write 0.5 mL, never .5 mL. A missing zero can make someone think it’s 5 mL instead of 0.5 mL. That’s a tenfold error.
- No trailing zeros: Write 5 mL, never 5.0 mL. The extra zero makes people think precision matters more than it does, and they might try to measure 5.0 when the device can’t do that.
- Space between number and unit: It should say 5 mL, not 5mL. That tiny space helps your brain separate the number from the unit.
A 2018 Johns Hopkins study showed that following these formatting rules cut 10-fold dosing errors by 47%. That’s not a small improvement-it’s life-saving.

Use the Right Measuring Tool
Never use a kitchen spoon, a medicine cup from last year, or a dropper unless it’s labeled with mL markings. The bottle should come with a dosing device: a syringe, a cup, or a spoon with mL lines. If it didn’t, ask for one. Pharmacies are required to give you a measuring tool that matches the label.
Look at the device. The lines should be clear and labeled in mL. Some go down to 0.1 mL for babies. Others only go to 1 mL. If your dose is 1.8 mL and your device only has 1 mL and 2 mL marks, you’re stuck. That’s why you need to ask for a syringe-those are the most accurate. A 5 mL syringe costs less than $1 and is far better than any cup.
One mother on Reddit said she used a kitchen spoon for three days because the cup that came with the medicine had faded lines. Her child was drowsy and unresponsive. She didn’t realize her spoon held 7 mL, not 5. That’s why you check the device before each dose. If the lines are blurry, get a new one.
What If the Label Is Confusing?
You’re not supposed to guess. If you’re unsure, call the pharmacy. Don’t wait. Don’t assume. Don’t Google it. Ask the pharmacist to explain it again-out loud.
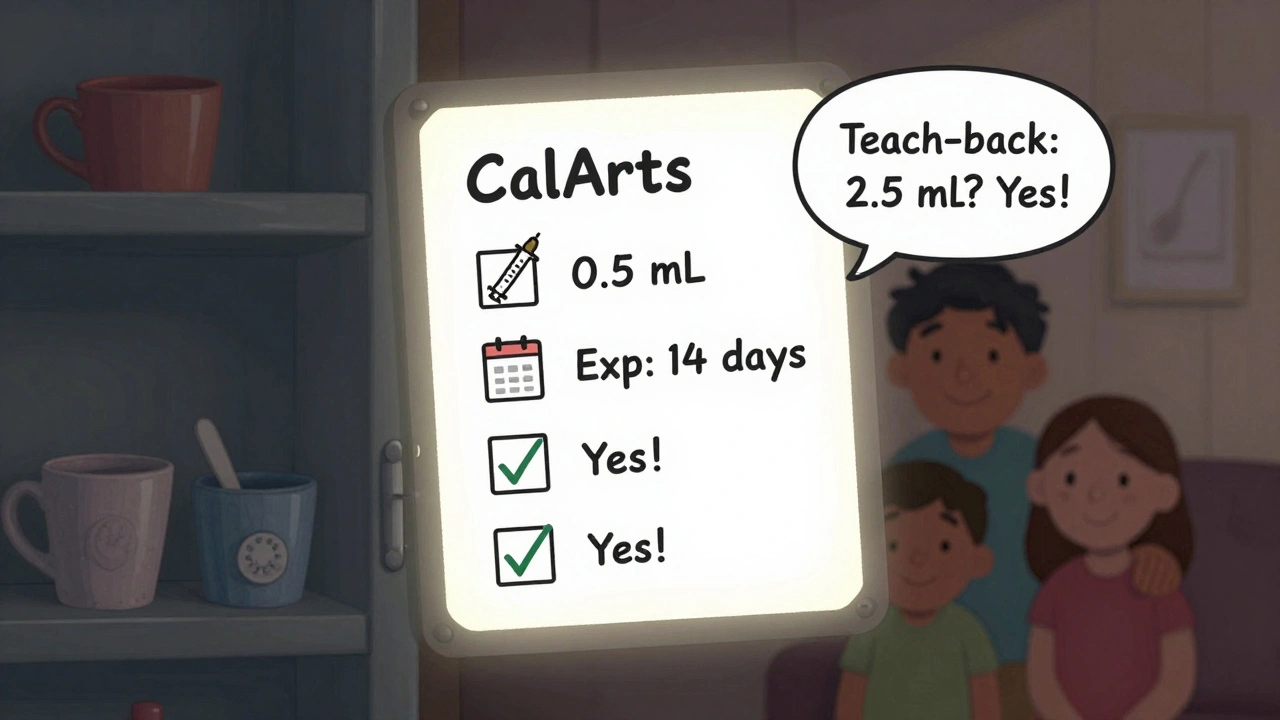
Use the teach-back method. After they explain, say: “So, if the label says 120 mg/5 mL and I need to give 60 mg, I give 2.5 mL?” If they say yes, you got it. If they hesitate, you didn’t. That simple check reduces errors by 63%, according to the Agency for Healthcare Research and Quality.
Also, check the expiration date. Liquid medicine can lose strength or grow bacteria after it expires. Most last 14 to 30 days after opening, unless the label says otherwise. Don’t use old medicine.
Why This Matters More for Kids
Children under 12 get 75% of all liquid prescriptions. Their bodies are smaller. A small mistake can have big consequences. That’s why the American Academy of Pediatrics now recommends that pediatricians talk about medication safety during every well-child visit.
Studies show that when parents get a live demonstration from a pharmacist, 78% get the dose right. Without it, the error rate jumps to 39.4%. That’s why you should always ask: “Can you show me how to measure this?” It takes two minutes. It could save a trip to the ER.
What’s Changing in 2025
By 2025, the FDA will start enforcing new rules. All liquid medication labels must have high-contrast text, minimum 10-point font, and pictograms showing how to use the dosing device. Some pharmacies are already testing QR codes that link to short videos-just scan it and see someone measure the dose correctly.
Amazon Pharmacy and McKesson’s Medly system already use these tools. They’ve seen 28% fewer calls about dosing confusion. That’s the future. But right now, the tools are still new. Your job is to use what’s available wisely.
Final Checklist Before Giving the Dose
- Is the dose written in mL? If not, ask for a corrected label.
- Is the number formatted correctly? 0.5 mL, not .5 mL or 5 mL.
- Do you have a proper measuring device? If not, ask for a syringe.
- Do you know the concentration? 120 mg/5 mL means 5 mL has 120 mg-not the whole bottle.
- Did you use the teach-back method? Repeat the dose back to the pharmacist.
- Is the medicine expired? Check the date.
Medication errors aren’t your fault. They’re built into a system that still uses confusing labels and unreliable tools. But you can protect yourself. Read the label. Use mL. Use the right tool. Ask questions. Don’t guess. That’s how you keep your family safe.
Can I use a kitchen spoon if the label says "1 teaspoon"?
No. Even if the label says "1 teaspoon," you should not use a kitchen spoon. Household spoons vary in size-some hold as little as 2.5 mL, others as much as 7.5 mL. That’s a 200% difference. Always use the measuring device that came with the medicine or ask the pharmacy for a syringe marked in mL.
What does 120 mg/5 mL mean on a liquid medicine label?
It means every 5 milliliters of the liquid contains 120 milligrams of the active drug. If your doctor prescribed 60 mg, you need to give half of that volume-2.5 mL-not 60 mL or half the bottle. Always calculate based on the concentration, not the total amount in the bottle.
Why is 0.5 mL written with a zero before the decimal?
Writing "0.5 mL" instead of ".5 mL" prevents dangerous mistakes. Without the leading zero, someone might misread it as "5 mL"-a tenfold overdose. This rule was created after studies showed it reduced fatal dosing errors by nearly half. Always look for the zero.
Is it okay to use an old medicine cup from a previous prescription?
No. Old cups may have faded lines, broken markings, or be the wrong size. Each prescription has a specific dose and device. Even if the cup looks similar, the measurements may not match. Always use the new device that comes with the current prescription-or ask for a syringe.
What should I do if the pharmacy didn’t give me a measuring device?
Ask for one. Pharmacies are legally required to provide a measuring device that matches the dose on the label. If they say they don’t have one, request a 5 mL oral syringe-they’re inexpensive, accurate, and easy to use. You can also buy them at any pharmacy or online for under $2.
Can I trust the dose if the label says "as directed"?
No. "As directed" is not a valid instruction on a prescription label. It’s a red flag. The label must clearly state the dose in mL and how often to give it. If it says "as directed," call the pharmacy and ask them to clarify the exact dose. Never guess.
How do I know if the medicine has gone bad?
Check the expiration date on the label. Most liquid medicines last 14 to 30 days after opening, unless the label says otherwise. Also look for changes in color, smell, or texture. If it looks cloudy, smells strange, or has particles floating in it, don’t use it. Return it to the pharmacy.
What to Do Next
If you’re caring for someone who takes liquid medicine, make this your new habit: always measure with a syringe, always check the concentration, always ask for clarification. Keep a small notebook next to the medicine cabinet. Write down each dose, time, and device used. It helps you spot patterns and catch mistakes early.
And if you ever feel unsure-even for a second-call the pharmacy. Don’t wait. Don’t hope. Don’t guess. The right dose isn’t just about following instructions. It’s about protecting someone you love.




Rachel Bonaparte
December 5, 2025 AT 13:45Okay, so let me get this straight-pharmacies are suddenly the guardians of truth in a world where Big Pharma is literally poisoning us with decimal-point deception? I’ve seen the FDA’s ‘guidelines’-they’re written by lobbyists who own shares in syringe manufacturers. That’s why they banned teaspoons. Not because spoons are dangerous, but because they want you dependent on their $2 plastic syringes that break after two uses. And don’t even get me started on QR codes-next they’ll be embedding tracking chips in the bottle caps. You think this is about safety? It’s about control. And you’re all just swallowing it-literally and figuratively.
Scott van Haastrecht
December 6, 2025 AT 13:12This entire post is a waste of bandwidth. You’re treating adults like children who can’t read a fraction. If you can’t tell 0.5 mL from 5 mL, you shouldn’t be medicating anyone. The real problem isn’t the label-it’s the people who refuse to think. Stop blaming the system. Take responsibility. Or stop having kids.
Michael Feldstein
December 7, 2025 AT 03:51Really appreciate this breakdown-it’s the kind of thing every parent needs to see before their first pediatric prescription. I used to wing it with kitchen spoons until my niece got a fever after an accidental overdose. Turned out my ‘teaspoon’ held 7 mL. The pharmacist laughed, then handed me a syringe and said, ‘This is your new best friend.’ Now I keep three on hand. One for each kid, one for emergencies, one for when I drop the first two. Seriously, if you’re measuring anything under 10 mL, use a syringe. It’s not expensive, it’s not complicated, and it’s the only way to be sure.
jagdish kumar
December 8, 2025 AT 15:56Measurement is an illusion. The body knows the truth. The label is just a shadow on the wall.
zac grant
December 10, 2025 AT 03:59Just ran through the checklist-99% of my patients miss #3 (measuring device) and #5 (teach-back). The syringe thing is non-negotiable. Even with clear labels, 42% of caregivers still use cups or spoons out of habit. The 10-fold error rate drops to 3% when you pair clear labeling with a syringe + verbal confirmation. It’s not magic-it’s systems design. Pharmacies need to hand out syringes like gum at the counter. If they don’t, escalate. It’s a legal obligation, not a favor.
Carolyn Ford
December 10, 2025 AT 09:56Heidi Thomas
December 10, 2025 AT 13:45Ashley Elliott
December 10, 2025 AT 19:29I want to say thank you for writing this. I’m a single mom of twins, and I’ve had two ER trips in two years because I misread a label. The first time, I thought ‘120 mg/5 mL’ meant the whole bottle had 120 mg. I gave them both the full dose. They were lethargic for hours. I didn’t know how to ask for help-I was too scared to sound stupid. This post is the kind of thing I wish I’d found two years ago. Please, if you’re reading this and you’re unsure-call the pharmacy. No one will laugh. I promise. I did. They were kind. And now I carry a syringe in my purse. Always.
Augusta Barlow
December 12, 2025 AT 14:45Look, I get it-labels are confusing. But let’s be real: the whole system is rigged. Why are we trusting a corporation to write our medicine instructions? Why aren’t we demanding independent oversight? Why do we have to learn ‘teach-back’ like it’s some kind of secret handshake? This isn’t about education-it’s about shifting blame onto the consumer. If the label was truly clear, why do we need a 10-point font mandate? Why do we need QR codes? Because the system failed. And now they’re asking us to fix it with a $2 syringe and a smile. I’m not buying it. The real solution? Ban liquid meds for kids. Use pills. Or better yet-don’t prescribe so much in the first place.
Chase Brittingham
December 13, 2025 AT 07:16Just wanted to say I’ve been a pharmacy tech for 12 years, and this is the most accurate summary I’ve seen. I’ve watched parents cry because they thought ‘1 tsp’ meant they could use their coffee spoon. I’ve held babies who overdosed because the cup had faded lines. We want to help. We’re not trying to confuse you. We’re trying to keep you alive. If you’re ever unsure, come in. We’ll show you. We’ll write it down. We’ll even draw you a picture. We’re not perfect, but we care. And you’re not alone in this.
Ollie Newland
December 13, 2025 AT 18:38Interesting piece. The metric standardization push is long overdue-especially in the US, where the imperial system still haunts medical practice. That said, the 2016 FDA ban on teaspoons was more symbolic than practical. Many rural pharmacies still print legacy labels due to outdated software. The real bottleneck isn’t patient literacy-it’s pharmacy IT infrastructure. If you’re getting a label with ‘tsp’, it’s not your fault. It’s a system failure. Push back politely. Ask for a digital copy. Most chains can email you a corrected version. And yes, syringes are still king. I keep a 5 mL one in my wallet. It’s saved my daughter twice.
Jordan Wall
December 14, 2025 AT 21:58OMG I literally just had this happen 😭 I gave my son 5mL thinking it was 0.5 because the 0 was too small and the 5 looked bold?? I thought it was 5mg not 5mL?? I panicked for 2 hours until I called the pharmacy and they were like ‘uh yeah that’s a 10x overdose’ and I just started crying. Now I have 3 syringes, a highlighter, and I read the label out loud to my cat before every dose. I’m not okay. But I’m safer. 🙏
Martyn Stuart
December 16, 2025 AT 00:27Brilliant. The leading zero rule alone prevents hundreds of pediatric deaths annually. I’ve trained over 300 caregivers in community clinics, and the single biggest improvement? Syringes + verbal confirmation. Also-don’t trust the ‘as directed’ line. It’s a red flag. If a prescription says that, it’s either a copy-paste error or the prescriber didn’t know the dose. Either way, call the pharmacy. Don’t wait. Don’t assume. Don’t Google. Just call. It’s 2 minutes. It could save a life. And yes-expired liquid meds are dangerous. I’ve seen mold grow in bottles left on bathroom counters. Don’t be that person.