SJS/TEN Symptom Checker
Critical Warning
STEVENS-JOHNSON SYNDROME AND TOXIC EPIDERMAL NECROLYSIS ARE MEDICAL EMERGENCIES. If you suspect SJS/TEN, stop the suspected medication immediately and go to the nearest emergency department. Do not wait.
Most people never think about their medication causing a life-threatening reaction. But for a small number of people, a common drug - like lamotrigine, allopurinol, or sulfamethoxazole - can trigger something far worse than a mild rash. It can be Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN), two sides of the same terrifying coin. These aren’t just bad skin reactions. They’re full-body emergencies that can kill. And they happen fast.
What Exactly Is SJS and TEN?
SJS and TEN are severe skin reactions caused by medications. They’re not allergies in the usual sense - no sneezing or hives. Instead, your skin starts to die. It begins with flu-like symptoms: fever, sore throat, burning eyes, fatigue. Within a few days, a painful red or purple rash spreads. Blisters form. Then your skin begins to peel off in sheets, like a bad burn. If it affects less than 10% of your body, it’s SJS. If more than 30% is involved, it’s TEN. Between 10% and 30%? That’s overlap syndrome - still dangerous.
Think of it like this: your skin isn’t just protecting you from the outside. It’s a living barrier that holds in fluids, keeps out germs, and regulates temperature. When SJS or TEN hits, that barrier collapses. You lose fluids. You get infections. Your eyes, mouth, and genitals start to erode. This isn’t something you wait out at home. It’s a hospital emergency - often in a burn unit or intensive care.
Which Medications Are Most Likely to Trigger It?
Not every drug causes this. But some are known red flags. The most common culprits include:
- Lamotrigine (used for epilepsy and bipolar disorder)
- Allopurinol (for gout)
- Carbamazepine and phenytoin (anti-seizure meds)
- Nevirapine (an HIV drug)
- Oxicam NSAIDs like meloxicam and piroxicam
- Sulfonamide antibiotics like sulfamethoxazole
- Phenobarbital
Here’s what makes it worse: if you’ve had SJS from one of these drugs before, you’re at extreme risk if you take it again - or even a similar one. Cross-reactivity is real. Someone who reacted to carbamazepine might also react to phenytoin or lamotrigine, even if they’ve never taken those before. That’s why survivors are told to avoid entire drug classes, not just the one that caused the problem.
And timing matters. Reactions usually start within the first 8 weeks of taking the drug - sometimes even after you’ve stopped it. For lamotrigine, restarting the drug after a break - even just a few days - can trigger SJS if you go back to the original dose. That’s why doctors stress slow dose increases and warn against skipping doses.
Who’s at Higher Risk?
It’s not random. Some people are more vulnerable:
- People with HIV or weakened immune systems
- Those taking sodium valproate with lamotrigine (a dangerous combo)
- People who’ve had a rash from epilepsy meds before
- Those allergic to trimethoprim
- People with a family history of SJS/TEN - there’s a strong genetic link, especially with certain HLA gene variants
- Children and young adults, though it can happen at any age
Genetics play a bigger role than most realize. For example, people of Asian descent with the HLA-B*15:02 gene are at much higher risk when taking carbamazepine. Some countries now test for this gene before prescribing it. In New Zealand, testing isn’t routine yet - but doctors should ask about family history and ethnicity when prescribing high-risk drugs.
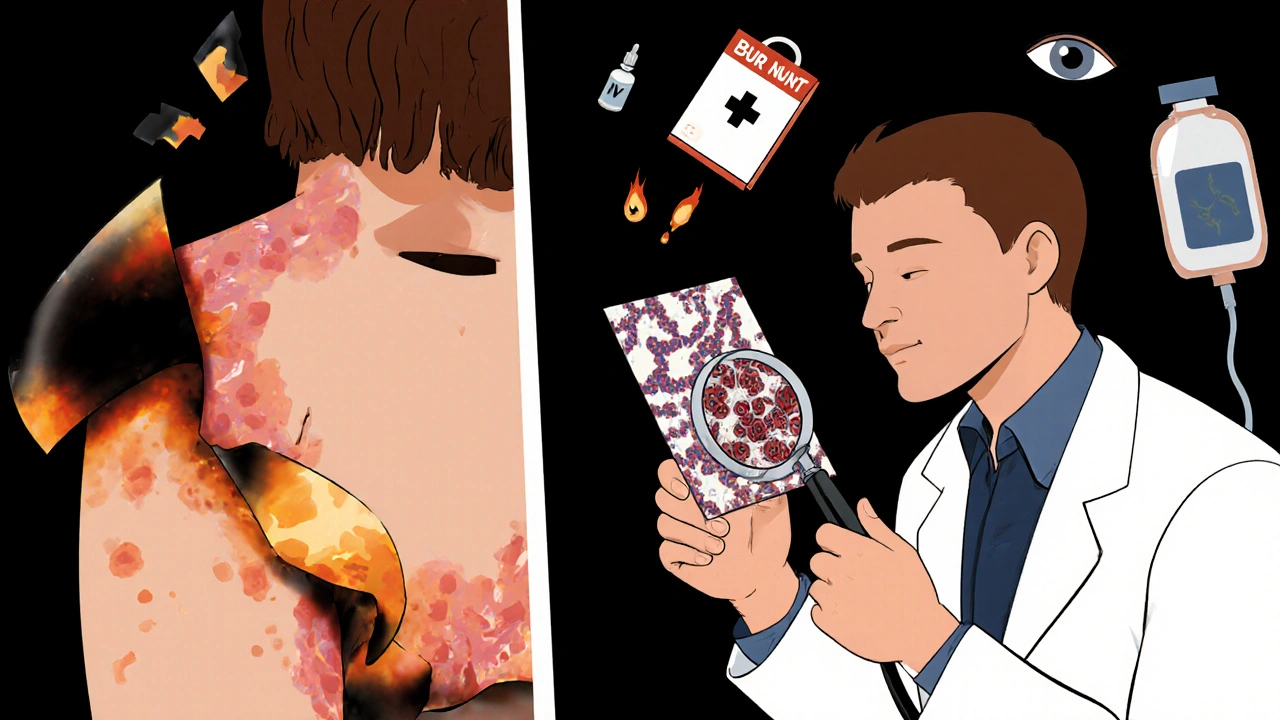
What Happens When It Hits?
The first sign? A fever that doesn’t go away. Then, burning eyes. A sore throat that feels like you’ve swallowed glass. A rash that spreads fast - not itchy, but painfully tender. Blisters form on your lips, inside your mouth, around your genitals. Your skin turns red, then blisters, then peels off in large patches. You might lose a fingernail or two. Your eyelids stick together. Swallowing becomes impossible. Your body starts to shut down.
Doctors confirm it with a skin biopsy. Under the microscope, they see full-thickness epidermal necrosis - the top layer of skin is dead, with little inflammation. That’s the hallmark. Blood tests and imaging help check for organ damage, but the skin tells the story.
And here’s the brutal truth: the longer you wait, the higher the chance you won’t survive. Mortality jumps from 5% in SJS to over 30% in TEN. Death usually comes from sepsis, organ failure, or massive fluid loss. Some people die from a pulmonary embolism or heart attack triggered by the stress on their body.
How Is It Treated?
There’s no magic cure. Treatment is about damage control.
- Stop the drug immediately. No exceptions. Even if you’re not sure, pull the plug.
- Get to a hospital - now. Emergency room. Don’t wait. Don’t call your GP. Go to A&E.
- Specialized care. Burn units are best. They know how to handle skin loss, fluid balance, and infection control.
- Supportive care. IV fluids, pain control, wound care, nutritional support. Your skin needs time to heal.
- Watch for complications. Eye damage is common. You’ll need daily eye exams. Mouth sores need special rinses. Urinary and genital areas must be monitored for scarring.
Some hospitals try immunomodulators like IVIG or corticosteroids, but the evidence is mixed. The best treatment? Early recognition and stopping the drug before it gets worse.
Long-Term Damage Is Real - And Often Overlooked
Survivors aren’t out of the woods. Many face lifelong problems:
- Blindness or severe vision loss in 30-50% of cases - from corneal scarring, dry eyes, or eyelids sticking shut
- Chronic dry mouth, gum disease, and tooth loss from mouth sores
- Scarring on skin, loss of pigment, or permanent nail damage
- Esophageal strictures - scar tissue making swallowing hard
- Vaginal stenosis in women, phimosis in men - scarring that affects sexual health
- Thinning hair or permanent hair loss
One woman in Auckland told her dermatologist she thought she was fine after 6 months. Then, at her yearly eye check-up, she found her cornea had scarred from untreated dryness. She lost 60% of her vision. She didn’t know her eyes needed daily drops for years. That’s why follow-up care with ophthalmologists, dermatologists, and dentists is non-negotiable.

Can It Be Prevented?
Yes - but only if you know the signs and act fast.
- If you’re prescribed lamotrigine, allopurinol, or any high-risk drug, read the warning leaflet. Keep it.
- Never start a new medication during the first 8 weeks of treatment unless your doctor says so.
- Never restart a drug after stopping it - especially lamotrigine - without your doctor’s guidance.
- If you get a rash, fever, or mouth sores while on these drugs, stop the medication and go to the hospital immediately.
- Tell your doctor if you or a family member has ever had SJS or a severe drug reaction.
Most rashes from these drugs are harmless. But if it spreads fast, hurts, or involves your mouth or eyes - don’t second-guess it. Go to the emergency department. Your life could depend on it.
What Should You Do If You Suspect SJS/TEN?
Here’s your quick action plan:
- Stop the suspected medication immediately.
- Call emergency services or go to the nearest hospital - do not wait.
- Take the medication bottle with you.
- Write down when symptoms started and what you’ve been taking.
- Don’t try to treat it at home. No creams, no antihistamines. This isn’t an allergic rash.
Doctors in emergency rooms see thousands of rashes. But they don’t always recognize SJS. Be persistent. Say: "I think this might be Stevens-Johnson Syndrome." That phrase gets attention.
Can Stevens-Johnson Syndrome be caused by vaccines?
No, SJS/TEN is almost always caused by medications - not vaccines. There are fewer than 10 documented cases worldwide linked to vaccines, and even those are debated. The overwhelming majority of cases come from drugs like lamotrigine, allopurinol, or antibiotics. Don’t avoid vaccines because of SJS fears - the risk is negligible.
Is SJS contagious?
No, SJS is not contagious. You can’t catch it from someone else. It’s a personal reaction to a drug, not an infection. But if you’re caring for someone with SJS, you need to protect yourself from infection - their skin is open, and they’re vulnerable to bacteria.
How long does recovery take?
Skin usually regrows in 2 to 4 weeks, but full recovery can take months or years. Many survivors deal with chronic dry eyes, pain, or scarring long after the rash is gone. Ocular complications can worsen over time if not monitored. Follow-up care isn’t optional - it’s essential.
Can you get SJS from over-the-counter painkillers?
Yes. Oxicam NSAIDs like piroxicam and meloxicam are known triggers. Even ibuprofen and naproxen have rare case reports, though they’re far less likely. If you develop a sudden rash with fever after taking any NSAID, stop it and seek help.
Are there genetic tests for SJS risk?
Yes - but only for specific drugs and populations. For example, people of Han Chinese, Thai, or Malaysian descent are tested for HLA-B*15:02 before taking carbamazepine. In New Zealand, testing isn’t standard unless you have Asian ancestry or a family history. If you’re prescribed a high-risk drug, ask your doctor if genetic testing is right for you.
What should I do if I’ve had SJS before?
Never take the drug that caused it again - and avoid all drugs in the same class. Tell every doctor, pharmacist, and dentist you’ve had SJS. Wear a medical alert bracelet. Keep a written list of all drugs you must avoid. Recurrence is common and often deadlier than the first time.
Final Thought: Know the Signs, Act Fast
SJS and TEN are rare. The chance of getting them is tiny - less than one in a million per week for even the riskiest drugs. But when it happens, it’s catastrophic. There’s no second chance to catch it early. If you’re on a high-risk medication and you feel off - fever, sore throat, burning eyes, a rash that spreads - don’t wait. Don’t check online. Don’t call your pharmacy. Go to the hospital. Your skin might be the first warning system your body has - and if you ignore it, you might not get another one.




Jessica Healey
November 17, 2025 AT 08:45I took lamotrigine for two years and never knew this could happen. My skin broke out one day like I’d been scalded-thought it was just stress. Turned out it was SJS. I spent 17 days in the burn unit. Don’t ignore a rash if it’s burning, not itching. This isn’t acne.
Gordon Mcdonough
November 18, 2025 AT 12:42OMG I JUST READ THIS AND I’M SHAKING-MY COUSIN DIED FROM THIS AFTER TAKING ALLOPURINOL AND NO ONE TOLD HIM! WHY ISN’T THIS ON EVERY PRESCRIPTION LABEL?! AMERICA’S HEALTHCARE IS A JOKE IF PEOPLE HAVE TO LEARN THIS THE HARD WAY!!
Levi Hobbs
November 18, 2025 AT 14:54This is one of the most important posts I’ve read in years. I’m a pharmacist, and I’ve seen too many patients dismissed when they report early symptoms. The key is timing-once blisters form, it’s already too late for most interventions. I now make it a point to verbally warn patients on high-risk meds, even if the leaflet says it. A quick 30-second chat can save a life.
Also, cross-reactivity is terrifying. Someone who reacted to carbamazepine shouldn’t touch lamotrigine-even if it’s ‘different.’ The immune system doesn’t care about drug class labels.
henry mariono
November 20, 2025 AT 07:12I had SJS after a course of sulfamethoxazole. I didn’t know what it was until my eyelids sealed shut. I’m lucky I made it. Now I wear a medical bracelet. I don’t talk about it much. But if you’re on any of these drugs and feel off-go to the ER. Don’t wait for a second opinion. Your body’s screaming.
Sridhar Suvarna
November 21, 2025 AT 02:16In India we rarely hear about this but it's real. My neighbor's son got TEN after taking ibuprofen for fever. He was 14. The doctors didn't recognize it for 48 hours. He lost 40% of his skin. He's alive but blind in one eye. This needs awareness everywhere. Not just in rich countries. Simple posters in pharmacies could save lives.
Also, don't assume OTC drugs are safe. They're not.
Joseph Peel
November 22, 2025 AT 03:07There’s a reason HLA-B*15:02 screening is mandatory in parts of Asia and not here. It’s not just about genetics-it’s about systemic neglect. We test for everything from BRCA to cystic fibrosis, but we won’t screen for a gene that prevents a 30% mortality rate? That’s not medical practice. That’s cost-cutting disguised as caution.
If you’re of Southeast Asian descent and prescribed carbamazepine, demand the test. Don’t let your doctor’s laziness be your death sentence.
Kelsey Robertson
November 22, 2025 AT 12:15Wow, another fear-mongering article that ignores the fact that 99.9999% of people take these drugs and never have this reaction. Why are we scaring people into avoiding life-saving meds? What’s next? ‘Don’t drink water-it might cause water intoxication!’
Also, if you’re so scared of SJS, why are you still using the internet? Maybe your phone’s EMF is triggering a latent immune collapse? Just a thought.
Joseph Townsend
November 23, 2025 AT 19:51Let me tell you something-SJS doesn’t just ruin your skin, it ruins your soul. I came out of that hospital with a new set of scars, a new fear of medicine, and a new hatred for doctors who think ‘it’s probably just a rash.’
My wife had to wipe my tears every morning for six months because my eyes were so dry they felt like sandpaper. I couldn’t eat anything crunchy. I couldn’t kiss my kid without pain. And the worst part? No one believed me when I said I was still suffering.
This isn’t a ‘rare side effect.’ It’s a silent killer that gets a footnote in a drug pamphlet. And we’re letting it happen.
Bill Machi
November 25, 2025 AT 05:50As someone who lost a brother to TEN after taking piroxicam, I can say this: the system failed him. He was told to ‘wait it out.’ He was given antihistamines. He was sent home. He died three days later.
There’s no excuse. Every prescriber of high-risk drugs should be required to watch a 10-minute video of SJS progression. Every pharmacy should have a laminated poster. Every patient should get a verbal warning and a printed checklist.
This isn’t ‘medical complexity.’ It’s negligence. And it’s preventable.