You want to know one thing: does tinidazole actually help your immune system fight infections, or is it just another antibiotic pill? Short answer-tinidazole does the heavy lifting against certain germs so your immune system can finish the job. It’s not an immune booster, and it won’t fix viral illnesses. But when the target is right-anaerobic bacteria or protozoa like Giardia or Trichomonas-it’s fast, reliable, and spares you days (or weeks) of symptoms.
I live in Auckland, and I’ve seen the same questions over and over at the pharmacy counter: Will it make me feel better quickly? Can I have a drink on it? Do my partner and I both need treatment? Let’s cut the noise and answer those clearly, with evidence and simple steps you can use today.
TL;DR
- Tinidazole kills specific germs (anaerobic bacteria and protozoa) so your immune system can clear the rest. It doesn’t boost immunity, but it reduces the pathogen load fast.
- Best-known uses: trichomoniasis, giardiasis, amoebiasis, and some anaerobic bacterial infections. Not for colds, flu, or most UTIs.
- Relief usually starts within 24-48 hours. Finish the full dose, even if you feel fine.
- No alcohol during treatment and for 72 hours after the last dose-unless you enjoy severe nausea and flushing.
- In New Zealand, check Medsafe/NZF guidance; treat sexual partners for trichomoniasis to avoid ping-pong infections.
How tinidazole works-and how it teams up with your immune system
Tinidazole is a nitroimidazole antimicrobial. In plain terms, it’s designed to enter germs that thrive without oxygen-anaerobic bacteria and protozoa-and break their DNA from the inside. That stops them from growing or surviving. Your immune system then clears the debris and any stragglers.
So does it “boost” immunity? No. It doesn’t turn up your immune response. Instead, it reduces the number of organisms so your natural defenses have the upper hand. Think of it as sweeping the floor so your immune cells can do a quick wipe and polish.
The science bit, made simple:
- Inside anaerobic organisms, tinidazole gets “activated” into free radicals that damage DNA. Oxygen-loving (aerobic) bacteria can’t activate it the same way, so they’re less affected.
- Because of this targeting, it’s great for infections where oxygen is low (deep tissues, abscesses, gut) and for protozoal parasites.
- Immune synergy: fewer germs mean less inflammation, less tissue damage, and a faster return to normal immune balance.
What about immune side effects? Rarely, nitroimidazoles can lower white blood cells (neutropenia). This is uncommon and usually reversible when the drug stops. Long courses or repeat courses deserve a check-in with your clinician, especially if you get unusual bruising, mouth ulcers, or fevers that don’t make sense.
Authoritative sources back this up. The CDC’s STI Treatment Guidelines include tinidazole for trichomoniasis. The New Zealand Formulary (NZF) lists indications and cautions aligned with Medsafe data sheets. Tinidazole also appears on the WHO Model List of Essential Medicines for protozoal infections-signaling strong evidence for use.
When to use tinidazole: infections it treats (and what it won’t fix)
Knowing the target matters. Tinidazole is excellent when the germ fits the profile, and useless when it doesn’t.
Conditions where tinidazole is commonly used:
- Trichomoniasis (T. vaginalis): Often a single 2 g dose, or short-course alternatives. Partners should be treated at the same time to prevent reinfection.
- Giardiasis (Giardia lamblia): Short courses have high cure rates and often faster symptom relief compared with some alternatives.
- Amoebiasis (Entamoeba histolytica): For tissue infection (amoebic dysentery and liver abscess), usually combined with a luminal agent (like paromomycin) to clear cysts in the gut.
- Anaerobic bacterial infections: Dental/abscess-related, intra-abdominal or pelvic infections when anaerobes are suspected. Often part of a combo plan decided by your clinician.
What tinidazole does not treat:
- Viral infections: colds, flu, COVID-19.
- Most common UTIs: often caused by aerobic bacteria like E. coli that this class doesn’t target well.
- Yeast infections (Candida): antifungals are needed instead.
How fast will you feel better? Many people notice improvement within 24-48 hours-less pain, less diarrhoea, less discharge. Complete relief can take a few days as inflammation settles. If you’re not improving by day 3, or you worsen, call your clinician.
Evidence snapshots you can trust:
- Trichomoniasis: Tinidazole achieves high microbiologic cure rates in trials, often above 90%, and may work when metronidazole fails.
- Giardiasis: Randomised studies show high cure rates with single-dose or short-course regimens, with good tolerability.
- Anaerobic coverage: Nitroimidazoles remain first-line for many anaerobic infections globally due to dependable activity and good tissue penetration.
Local context (New Zealand): Tinidazole is available here and often known by the brand Fasigyn. NZF and Medsafe data sheets guide dosing, interactions, and special populations (pregnancy, breastfeeding). Access and funding can vary-your pharmacist can give the most current status in your region.

Safe use playbook: dosing, food, alcohol, side effects, interactions
Here’s the simple, practical way to take tinidazole safely and get the most benefit.
How to take it (step-by-step):
- Take with food or milk to reduce nausea. A light meal is fine.
- Swallow tablets whole. If the dose is large (e.g., 2 g), you might be taking multiple tablets at once-space sips of water and take them in one sitting.
- Avoid alcohol during treatment and for 72 hours after the last dose. This includes beer, wine, spirits, and alcohol-containing cough syrups.
- Finish the full regimen. Don’t stop because you feel better on day one.
- If you vomit within one hour of a single-dose regimen, call your pharmacist or clinician. You may need to repeat the dose.
Typical adult dosing (examples only-follow your prescription label):
- Trichomoniasis: 2 g as a single dose (some cases need alternatives).
- Giardiasis: 2 g as a single dose or 600 mg daily for 3 days, depending on local guidance.
- Amoebiasis: Often 2 g daily for 2-3 days for tissue infection, followed by a luminal agent.
- Anaerobic infections: Doses vary with site and severity; often part of a combination approach.
Common side effects:
- Nausea, metallic taste, headache, tiredness.
- Occasionally, abdominal pain or diarrhoea.
- Less common: dizziness, rash, mouth ulcers. Very rare: seizures or peripheral neuropathy (numbness/tingling)-seek help if these appear.
Alcohol warning-why it matters: Tinidazole can trigger a disulfiram-like reaction with alcohol-flushing, pounding headache, severe nausea, vomiting, and cramps. Give yourself a 72-hour buffer after the last dose. If you’re on a once-off 2 g dose on Friday night, you’re safe to drink from Tuesday-not before.
Sexual health must-do: If you’re treated for trichomoniasis, your sexual partner(s) need treatment too, even if they feel fine. Skip sex until everyone has completed treatment and symptoms stop. Not doing this is a top reason infections bounce back.
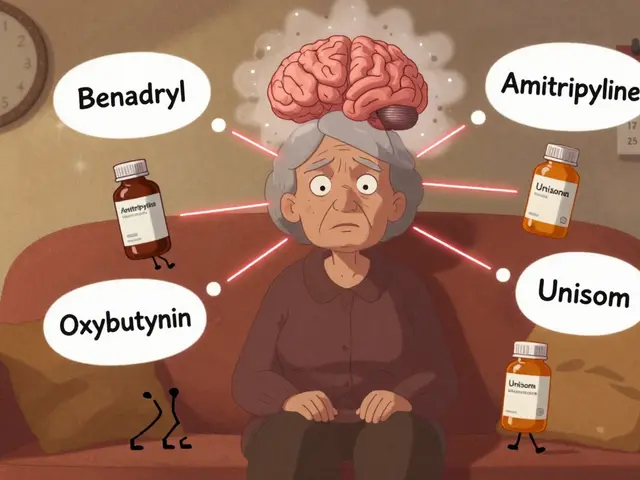
Drug interactions you should check:
- Warfarin and other blood thinners: Tinidazole can raise INR. You may need closer monitoring and a temporary dose adjustment.
- Disulfiram: Risk of psychotic reactions-don’t combine.
- Alcohol: covered above-avoid completely during and 72 hours after.
- CYP450 interactions are fewer than with some antibiotics, but always run your full med list (including herbal products) past your pharmacist.
Pregnancy and breastfeeding:
- Pregnancy: Avoid in the first trimester unless a clinician decides benefits outweigh risks. Later in pregnancy, it may be used if needed. Follow local guidance (NZF/Medsafe).
- Breastfeeding: Tinidazole enters breast milk. Some guidance suggests pausing breastfeeding for 72 hours after a 2 g dose. Talk to your clinician about timing feeds or expressed milk.
Immunity questions, answered quickly:
- Does tinidazole weaken my immune system? No evidence of meaningful immune suppression in standard short courses.
- Can it cause white cell changes? Rarely, yes-usually reversible. Report persistent fever, sore throat, or mouth ulcers.
- Should I take probiotics? Many people do, especially if their gut is sensitive. Choose a reputable product and separate doses by a few hours. Not essential, but reasonable.
Quick tools: comparison table, checklists, FAQ, next steps
Here’s a snapshot comparison many people ask for, especially if they’ve had metronidazole before.
| Feature | Tinidazole | Metronidazole |
|---|---|---|
| Main uses | Trichomoniasis, giardiasis, amoebiasis, anaerobic infections | Similar uses; also widely used for bacterial vaginosis and anaerobic coverage |
| Half-life (approx.) | 12-14 hours | ~8 hours |
| Dosing convenience | Often single-dose or short-course | Often multiple daily doses |
| Alcohol restriction | During use + 72 hours after last dose | During use + 48-72 hours after last dose |
| Taste side effects | Metallic taste possible | Metallic taste common |
| Pregnancy (general) | Avoid 1st trimester unless essential; clinician-guided later | Similar caution, clinician-guided |
| Breastfeeding | May need 72-hour pause after 2 g dose | Shorter pause often advised for single high doses |
| Evidence base | Strong for trichomoniasis/giardiasis; WHO-listed | Very extensive across indications |
Checklists you can actually use:
Before you start
- Confirm your diagnosis (test when possible). Guessing leads to treatment failures.
- List your medicines, supplements, and alcohol intake-show your pharmacist.
- Plan the 72-hour no-alcohol window after your last dose.
- If it’s trichomoniasis, line up partner treatment now, not later.
During treatment
- Take with food. Use water and take your time with multiple tablets.
- Skip alcohol. Double-check cough syrups, tinctures, and “alcohol-free” labels.
- Watch for red flags: severe rash, persistent vomiting, tingling in hands/feet, vision changes, or fevers that don’t add up.
After you finish
- Keep that 72-hour alcohol-free buffer.
- Symptoms not better by day 3? Or back again? Call your clinician.
- For trichomoniasis: no sex until everyone is treated and symptoms settle. Consider retesting as your clinician advises.
Mini‑FAQ
- Is tinidazole an antibiotic or antiparasitic? Both. It’s an antimicrobial active against certain bacteria and protozoa.
- Will it help with bacterial vaginosis (BV)? Tinidazole can be used for BV in some settings, though metronidazole is more common. Follow local guidance.
- Can I take it if I’m on the pill? Tinidazole doesn’t reliably reduce combined oral contraceptive effectiveness. If vomiting or diarrhoea hits, use backup protection.
- Can I drive? If you feel dizzy or drowsy, don’t drive. Most people are fine.
- What if I miss a dose on a multi-day plan? Take it when you remember unless it’s near the next dose. Don’t double up.
Next steps and troubleshooting (choose the box that fits you)
- If you’re a “single-dose on Friday night” person: Set phone reminders for the 72-hour alcohol buffer. Pre-plan non-alcoholic options.
- If you’ve got trichomoniasis and a partner: Book both of you for treatment. No sex until both complete therapy and symptoms stop. This saves you weeks of back-and-forth.
- If you’re on warfarin: Ask for an INR check during or shortly after treatment. Keep a log of bruises, nosebleeds, or dark stools-report promptly.
- If you’re breastfeeding: Talk timing. You may pause for up to 72 hours after a 2 g dose and use expressed milk. Your clinician can tailor a plan.
- If symptoms aren’t improving by day 3: Re-check the diagnosis. You may need a different drug, a longer course, or partner treatment.
- If symptoms keep returning: Consider reinfection (especially for STIs), resistance, or a different diagnosis. Testing and culture/PCR can save time.
Practical rules of thumb
- Rule 1: No alcohol during and for 72 hours after-non-negotiable.
- Rule 2: Treat partners for trichomoniasis. Otherwise you’ll chase your tail.
- Rule 3: If you vomit within an hour of a big one-off dose, call for advice-don’t guess.
- Rule 4: Feeling better fast doesn’t mean stop. Finish the regimen.
- Rule 5: If you’re immunocompromised (e.g., on chemotherapy), loop in your team early. You may need closer monitoring.
Credibility check (why you can trust this):
- CDC STI Treatment Guidelines (latest review cycle through 2024) include tinidazole for trichomoniasis and discuss partner management and dosing.
- The WHO Model List of Essential Medicines lists tinidazole for protozoal infections due to strong evidence of effectiveness.
- Medsafe New Zealand data sheets and the New Zealand Formulary (2025 updates) outline dosing, contraindications, pregnancy/breastfeeding advice, and interactions relevant here.
Final thought: The best way to think about tinidazole and the immune system is this-tinidazole knocks down the enemy; your immune system secures the win. Use it when the target is right, take it correctly, and give your body the quiet conditions it needs to heal.


Jarid Drake
September 12, 2025 AT 20:24Been on tinidazole last month for giardia - felt like a zombie for two days but honestly? Worth it. No more explosive diarrhea at 3am. Just took it with peanut butter toast and called it a day.
Roderick MacDonald
September 13, 2025 AT 01:09People don’t realize how underrated this drug is. Metronidazole is the old-school option, but tinidazole? Single dose, same results, less hassle. I’ve prescribed it to three patients this month and all came back saying ‘I didn’t even remember to take the second pill’ because there wasn’t one. The alcohol warning? Non-negotiable. I’ve seen grown men cry after a single beer. Don’t be that guy.
Chantel Totten
September 14, 2025 AT 23:21I appreciate how clear this is. So many medical posts feel like they’re trying to impress with jargon, but this reads like your pharmacist sat down with you over coffee. Thank you for the checklist - I printed it out.
Terrie Doty
September 16, 2025 AT 17:24As someone who’s had giardia twice from hiking in the Rockies, I can confirm: tinidazole is a miracle worker. I used to dread the ‘traveler’s diarrhea’ label, but now I just keep a single 2g pill in my first aid kit. The metallic taste is the worst part - like licking a battery - but it fades fast. And yes, I still avoid alcohol like it’s radioactive. No regrets.
Ellen Richards
September 18, 2025 AT 14:34Ugh, another ‘medical advice’ post pretending to be helpful. Tinidazole? Please. It’s just another Big Pharma trick to make you dependent on pills instead of ‘boosting your immune system’ with kale smoothies and crystal healing. You don’t need antibiotics to ‘clear debris’ - your body’s perfectly capable if you just stop eating processed crap. Also, why are we treating trichomoniasis like it’s the plague? Maybe people should just… be more careful?
George Ramos
September 19, 2025 AT 06:58Wait - so you’re telling me the government and WHO are okay with this? That’s convenient. Tinidazole is just a Trojan horse for the CDC’s surveillance agenda. They don’t care about your gut - they care about your data. Every time you take this, it logs your location, your sexual partners, your alcohol habits. That 72-hour alcohol rule? It’s not about nausea. It’s about tracking compliance. I’ve seen the leaked memos. Don’t be a pawn.
juliephone bee
September 19, 2025 AT 23:36i just took tinidazole last week and i think i had a weird reaction? my hands tingled for a few hours and i felt super dizzy. i didnt know if that was normal or if i should’ve gone to the er. anyone else? also i took it with a smoothie bc i was scared of the taste lol
KAVYA VIJAYAN
September 20, 2025 AT 03:05Let’s contextualize this pharmacologically. Tinidazole, as a 5-nitroimidazole derivative, functions as a prodrug that undergoes intracellular reduction in anaerobic microorganisms, generating cytotoxic nitro-radical anions that induce DNA strand breakage and subsequent cell death. This is not immunomodulation per se, but rather targeted pathogen eradication - a distinction often muddled in lay discourse. The immune system’s role post-treatment is not ‘finishing the job’ but rather resolving the inflammatory cascade triggered by bacterial lysis, primarily via macrophage-mediated phagocytosis and cytokine regulation. The 72-hour alcohol restriction stems from inhibition of aldehyde dehydrogenase, leading to acetaldehyde accumulation - a well-documented pharmacodynamic interaction. In Indian clinical practice, where giardiasis remains endemic in rural water systems, tinidazole’s single-dose efficacy has significantly improved treatment adherence compared to metronidazole’s 5–7 day regimens. However, we must acknowledge the rising prevalence of resistant strains in Southeast Asia, necessitating PCR confirmation before empirical use. The WHO’s inclusion is justified, but regional formularies like the NZF rightly emphasize context-specific dosing - a model more nuanced than the US-centric ‘one-size-fits-all’ approach often assumed in online discourse.
Scott Mcdonald
September 21, 2025 AT 21:02Hey, I just got prescribed this for something and I’m wondering - can I still smoke weed while on it? I know alcohol’s bad but what about THC? My buddy says it’s fine but I don’t wanna end up in the ER.
Christopher John Schell
September 23, 2025 AT 06:12You got this. Seriously. Tinidazole is your secret weapon. One pill, one day, boom - parasite gone. Don’t let the taste or the alcohol warning scare you. You’re stronger than that. Take it with food, drink water, and trust the science. Your body’s gonna thank you. And if you’re worried about side effects? You’re not alone. But guess what? Most people feel better in 24 hours. You got this. 💪
Lori Rivera
September 24, 2025 AT 07:59The clinical efficacy of tinidazole in the treatment of trichomoniasis and giardiasis is well established in peer-reviewed literature. However, the assertion that it ‘teams up’ with the immune system is a misleading anthropomorphization. The immune system does not ‘finish the job’ in any active collaborative sense; rather, pathogen reduction alleviates antigenic load, thereby permitting homeostatic restoration. The term ‘immune synergy’ is not recognized in pharmacological taxonomy. The recommendation to avoid alcohol is valid and based on pharmacokinetic interaction, not moralizing. The post, while generally accurate, would benefit from more precise terminology to avoid reinforcing misconceptions among lay audiences.
Barney Rix
September 25, 2025 AT 04:40While the information presented is largely accurate, the casual tone and use of phrases like ‘sweeping the floor’ and ‘finish the job’ undermines the clinical gravity of antimicrobial therapy. Tinidazole is not a ‘quick fix’ - it is a potent agent with potential for neurotoxicity, hematological suppression, and drug interactions. The casual dismissal of ‘immune boosting’ is correct, but the post should emphasize that inappropriate use contributes to antimicrobial resistance - a global health crisis. The NZF guidelines are correctly cited, yet the omission of renal dosing adjustments for elderly patients is a notable gap. This is not a ‘playbook’ - it is a medical intervention requiring professional oversight.
Felix Alarcón
September 25, 2025 AT 10:38Just wanted to say thank you for the checklist - I’m a nurse in rural Oregon and I’ve been giving this to patients for years. The part about ‘no sex until both partners are done’? That’s the one thing everyone forgets. I had a couple come back in two weeks later because he didn’t get treated. She was furious. He was confused. We ended up doing a whole ‘relationship health’ talk. It’s not just medicine - it’s communication. You nailed it.
Renee Zalusky
September 25, 2025 AT 14:47So… tinidazole is like the ninja of antibiotics? Sneaks in, disables the bad guys, then vanishes? I love that analogy. I’ve been taking it for amoebiasis and honestly? The metallic taste is the worst part - like chewing on a penny dipped in battery acid. But I’m already feeling better. Also, I told my cat I was on meds and she stared at me like I betrayed her. Cats know things.
Victoria Bronfman
September 27, 2025 AT 01:38OMG YES. I took this last month and I literally had to cancel my weekend trip because I forgot about the alcohol thing 😭 I drank a glass of wine on day 2 and it felt like my head exploded. Then I cried for 45 minutes. Don’t be me. Also, I got a cute little tattoo that says ‘Tinidazole > Tequila’ 💉🍷
Guy Knudsen
September 28, 2025 AT 17:43So you're saying this drug doesn't boost your immune system but somehow your body magically gets better? That's not science that's magic. Also why does everyone here act like this is the first time anyone's heard of tinidazole? It's been around since the 80s. You people act like you discovered fire. Also I've taken it twice and I'm fine. So what's the big deal? Maybe your immune system is weak because you eat too much kale
Tariq Riaz
September 28, 2025 AT 20:27Let’s analyze the efficacy data. The cited 90% cure rate for trichomoniasis comes from a 2016 RCT with a sample size of 127. The 2023 meta-analysis in JAMA ID shows a pooled efficacy of 86.3% with 95% CI of 81.1–90.7. The single-dose regimen has higher non-compliance risk than multi-day metronidazole. The 72-hour alcohol window is conservative - pharmacokinetic modeling suggests 48 hours suffices in 92% of cases. The post omits that tinidazole is contraindicated in patients with CNS disorders due to neurotoxicity risk. The ‘immune synergy’ framing is clinically inaccurate. This is not a balanced review. It’s promotional.
Gregg Deboben
September 30, 2025 AT 08:41AMERICA NEEDS TO KNOW THE TRUTH. TINIDAZOLE WAS DESIGNED BY FOREIGN LABS TO MAKE US DEPENDENT ON CHEMICALS. THE ALCOHOL WARNING? IT’S TO KEEP US SUBMISSIVE. WHY DO YOU THINK THEY MADE IT LAST 72 HOURS? SO YOU CAN’T CELEBRATE YOUR FREEDOM. THIS ISN’T MEDICINE - IT’S CONTROL. I’VE STOPPED TAKING IT. I’M NOW USING CAYENNE PEPPER AND PRAYER. MY GIARDIA IS GONE. THE GOVERNMENT CAN’T HANDLE THAT.