HIV Protease Inhibitor Comparison Tool
Select a Drug to Compare
Click on one of the buttons above to view detailed information about each protease inhibitor.
| Characteristic | Indinavir | Atazanavir | Darunavir | Lopinavir/Ritonavir | Saquinavir |
|---|---|---|---|---|---|
| Approval Year | 1997 | 2003 | 2006 | 2000 | 1995 |
| Dosing Frequency | Twice daily | Once daily | Once daily | Twice daily | Twice daily |
| Food Requirement | Empty stomach | Low-fat meal | With or without food | With or without food | High-fat meal |
| Typical Cost (USD/month) | $1,200 | $900 | $1,100 | $800 | $950 |
| Notable Side Effects | Kidney stones, hyperbilirubinemia | Jaundice, mild GI upset | Diarrhea, rash | Hypertriglyceridemia, GI intolerance | Metabolic changes, taste alteration |
Important Considerations
When selecting a protease inhibitor, consider factors such as:
- Renal Function: Indinavir carries a significant risk of kidney stones; newer agents are safer for patients with CKD.
- Dosing Convenience: Once-daily regimens reduce pill burden and improve adherence.
- Drug Interactions: Some drugs may interact with antacids or affect lipid metabolism.
- Resistance Profile: Darunavir remains active against many resistant strains.
Quick Summary
- Indinavir is an older HIV protease inhibitor with twice‑daily dosing but notable kidney stone risk.
- Modern alternatives like atazanavir, darunavir and lopinavir/ritonavir offer once‑daily dosing and fewer renal side effects.
- When choosing, consider resistance profile, drug‑food interactions, pill burden and cost.
- For patients with chronic kidney disease, newer agents are generally safer.
- All options require combination with other antiretrovirals to achieve full viral suppression.
What is Indinavir?
When treating HIV, Indinavir is a protease inhibitor that blocks the HIV‑1 protease enzyme, preventing the virus from maturing into infectious particles. Marketed under the brand name Crixivan, it received FDA approval in 1997.
Key attributes:
- Typical dose: 800mg taken twice daily, preferably on an empty stomach.
- Drug class: Protease inhibitor (PI).
- Common side effects: Crystalluria, hyperbilirubinemia, lipodystrophy, and mild nausea.
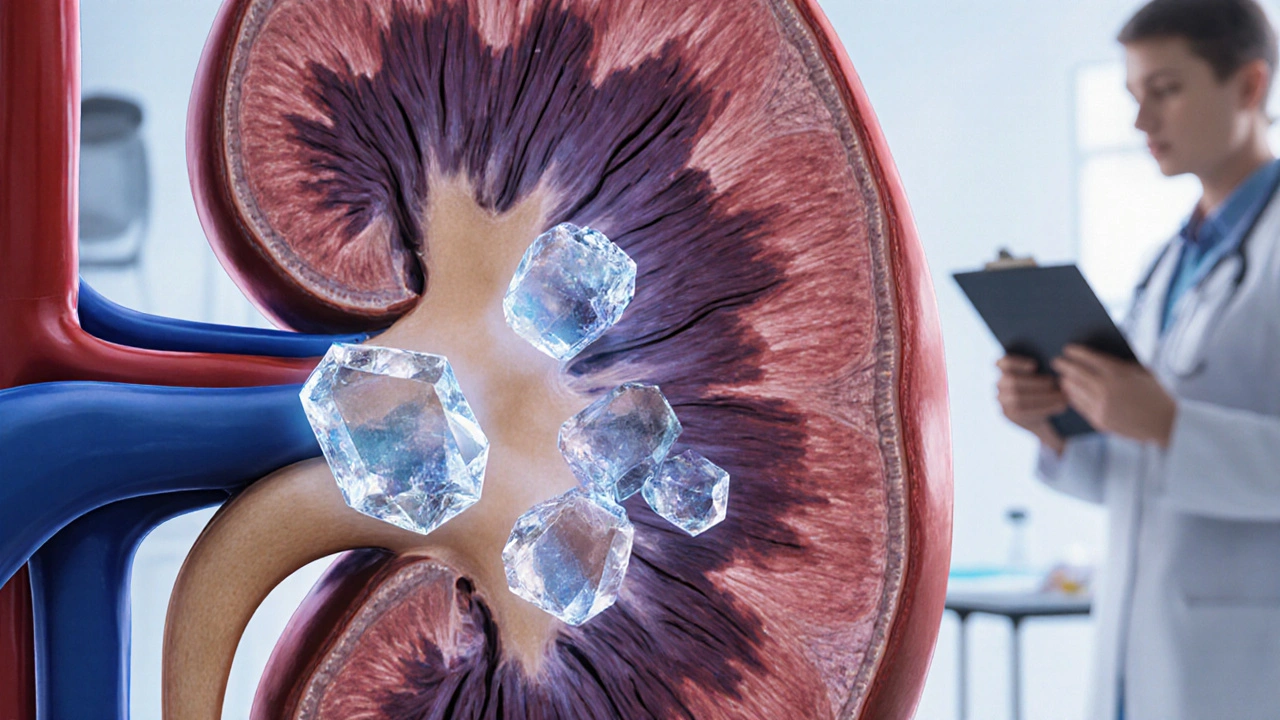
- Major safety concern: Indinavir can precipitate in the urinary tract, leading to kidney stones in up to 10% of patients.
- Cost (2025 US average): Approximately $1,200 per month for generic formulation.
Indinavir’s efficacy is well documented, achieving viral load suppression comparable to newer PIs when paired with a robust backbone regimen. However, its dosing frequency and renal risks have pushed clinicians toward alternatives for most patients today.
Modern Protease Inhibitor Alternatives
The HIV treatment landscape now includes several next‑generation protease inhibitors that improve convenience and safety. Below are the most widely used alternatives.
Atazanavir, often combined with ritonavir (boosted atazanavir), was approved in 2003. It can be taken once daily with a low‑fat meal.
Darunavir entered the market in 2006. When boosted with ritonavir or cobicistat, it allows once‑daily dosing and retains activity against many PI‑resistant strains.
Lopinavir/ritonavir (Kaletra) is a fixed‑dose combination approved in 2000. It is taken twice daily but has a well‑known tolerability profile.
Saquinavir, another early PI, is now mostly used in its boosted form (Saquinavir/ritonavir) and requires administration with a high‑fat meal to improve absorption.
Side‑by‑Side Comparison
| Drug | Brand (if any) | FDA approval | Dosing frequency | Food requirements | Typical cost (US$/month) | Notable side effects |
|---|---|---|---|---|---|---|
| Indinavir | Crixivan | 1997 | Twice daily | Empty stomach (1h before or 2h after meals) | ~$1,200 (generic) | Kidney stones, hyperbilirubinemia |
| Atazanavir (boosted) | Reyataz | 2003 | Once daily | Low‑fat meal | ~$900 (generic) | Jaundice, mild GI upset |
| Darunavir (boosted) | Prezista | 2006 | Once daily | Can be taken with or without food | ~$1,100 (generic) | Diarrhea, rash |
| Lopinavir/ritonavir | Kaletra | 2000 | Twice daily | With or without food | ~$800 (generic) | Hypertriglyceridemia, GI intolerance |
| Saquinavir (boosted) | Invirase | 1995 (boosted 2003) | Twice daily | High‑fat meal | ~$950 (generic) | Metabolic changes, taste alteration |
Pros and Cons by Drug
Indinavir
Pros: Proven efficacy, lower cost for brand‑name generic, minimal CYP3A4 interactions.
Cons: Twice‑daily schedule, strict fasting requirement, high risk of renal calculi, requires adequate hydration.
Atazanavir (boosted)
Pros: Once‑daily dose, less impact on lipid profiles, tolerable in patients with cardiovascular risk.
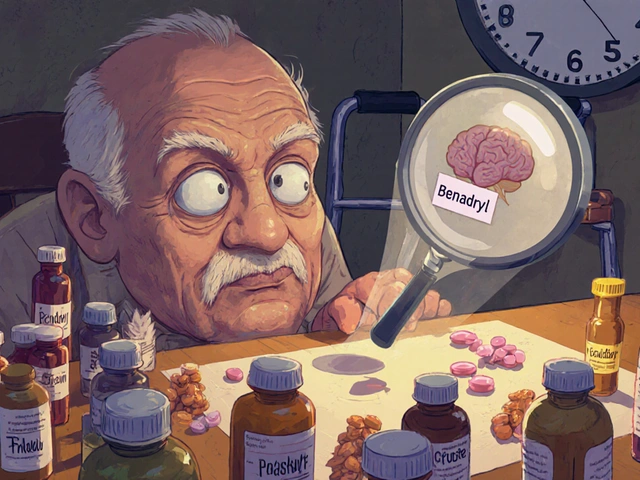
Cons: Can cause indirect hyperbilirubinemia (jaundice), modest drug‑drug interaction with antacids.
Darunavir (boosted)
Pros: Strong activity against PI‑resistant HIV strains, flexible with food, once‑daily option available.
Cons: Requires boosting agent, potential for increased serum creatinine, higher pill burden when boosted.
Lopinavir/ritonavir
Pros: Widely studied, often used in pediatric formulations, robust barrier to resistance.
Cons: Twice‑daily dosing, notable impact on triglycerides and cholesterol, frequent GI side effects.
Saquinavir (boosted)
Pros: Useful when other PIs are contraindicated, effective in some salvage regimens.
Cons: Requires high‑fat meal for absorption, twice‑daily schedule, metabolic side effects.
How to Choose the Right Protease Inhibitor
Picking a PI isn’t a “one‑size‑fits‑all” decision. Here’s a quick decision framework:
- Renal function: If eGFR<60mL/min/1.73m², avoid Indinavir because of stone risk.
- Resistance profile: For patients with prior PI exposure, darunavir offers the broadest coverage.
- Pill burden & lifestyle: Once‑daily options (atazanavir, darunavir) improve adherence for busy schedules.
- Metabolic concerns: Atazanavir has the mildest impact on lipids; lopinavir/ritonavir can raise triglycerides substantially.
- Cost considerations: Generic Indinavir remains the cheapest, but insurance formularies may favor newer generics with better safety.
- Drug‑food interactions: Assess whether the patient can consistently take a high‑fat or low‑fat meal as required.
In practice, many clinicians start with a boosted atazanavir or darunavir regimen for treatment‑naïve patients, reserving Indinavir for specific cases where cost constraints outweigh its drawbacks.
Monitoring and Managing Side Effects
Regardless of the chosen PI, regular monitoring is key.
- Kidney function: Serum creatinine and urine analysis every 3‑6months for Indinavir users.
- Liver function: Bilirubin and transaminases quarterly when using atazanavir.
- Lipid panel: Fasting lipids at baseline and then annually, more frequently if on lopinavir/ritonavir.
- Adherence checks: Pharmacy refill data or patient self‑report to catch missed doses early.
If side effects emerge, clinicians can switch to an alternative PI without compromising the overall regimen, provided resistance testing supports the change.
Frequently Asked Questions
Is Indinavir still prescribed in 2025?
Yes, but primarily for patients who need a low‑cost option and have no significant renal issues. Many clinicians prefer newer PIs for their safety and convenience.
Can I take Indinavir with food?
Indinavir must be taken on an empty stomach-at least 1hour before or 2hours after a meal-to avoid reduced absorption and higher risk of crystal formation.
What is the main advantage of atazanavir over Indinavir?
Atazanavir offers once‑daily dosing, fewer renal side effects, and a lower impact on cholesterol, making it easier for long‑term adherence.
Do boosted protease inhibitors increase drug interactions?
Boosting agents (ritonavir or cobicistat) inhibit CYP3A4, so they can raise levels of many co‑administered drugs. A thorough medication review is essential when prescribing boosted regimens.
How often should viral load be checked after switching PIs?
Guidelines recommend measuring plasma HIV‑1 RNA at 4weeks post‑switch, then at 12weeks, and subsequently every 3-6months if the patient remains suppressed.





Jay Ram
October 6, 2025 AT 15:21Yo folks, just skimmed through this massive comparison and thought I’d drop a quick take. Indinavir’s old‑school vibe is still solid in terms of raw potency, but the twice‑daily schedule and that dreaded kidney stone risk can be a real pain. The newer PIs like atazanavir and darunavir really shine with once‑daily dosing, making life easier for anyone juggling a busy schedule. Cost‑wise, Indinavir isn’t the cheapest anymore, especially when you factor in the generic competition. Overall, if you’ve got good renal function and don’t mind the fasting rule, it can still be a decent option. Otherwise, I’d say check out the newer agents for a smoother ride.
Elizabeth Nicole
October 7, 2025 AT 10:48Hey everyone! I dug a bit deeper into the side‑effect profiles and found that the hyperbilirubinemia with atazanavir is usually benign, whereas Indinavir’s kidney stones can actually require surgical intervention if you’re unlucky. Also, the food requirements are pretty different – Indinavir wants an empty stomach, atazanavir only a low‑fat snack, and darunavir is pretty flexible. If you’re looking at adherence, a once‑daily pill beats a twice‑daily regimen any day. For those on a tight budget, the generic price gap isn’t huge, but the hidden costs of monitoring kidney function with Indinavir can add up.
Dany Devos
October 8, 2025 AT 06:14From a methodological standpoint, the presented table adheres to standard comparative frameworks, yet it omits crucial pharmacokinetic parameters such as Cmax and AUC values, which are indispensable for a rigorous evaluation. Moreover, the discussion fails to address the impact of CYP3A4 polymorphisms on drug metabolism, particularly pertinent for atazanavir and darunavir. The omission of longitudinal adherence data also limits the practical applicability of the comparison. While cost estimates are useful, they do not reflect patient assistance programs that may substantially reduce out‑of‑pocket expenses. In summary, the analysis is a solid starting point but requires augmentation with deeper clinical pharmacology insights.
Sam Matache
October 9, 2025 AT 01:41Alright, picture this: Indinavir is the drama queen of the 90s, still trying to steal the spotlight while the newer PIs are chilling on the red carpet, sipping espresso and telling it like it is. Twice‑daily dosing? That’s like asking someone to floss after every meal – nobody’s got time! And the kidney stone saga? Pure melodrama. Meanwhile, atazanavir walks in with a single pill, low‑fat snack in hand, whispering, “I got you, fam.” The whole thing feels like a soap opera that finally found its happy ending with the once‑daily cast. 🎭
Hardy D6000
October 9, 2025 AT 21:08Look, as an American we should champion the drugs that keep our healthcare costs low, and Indinavir’s generic price is a testament to that. The so‑called kidney stone risk is overblown – just stay hydrated, drink water, and you’re fine. Why bother switching to fancy foreign meds that cost more and require special meals? The US system gave us the freedom to pick a cheap, effective PI, and we should stick with it. Don’t let the global elite push their pricey alternatives on us.
Amelia Liani
October 10, 2025 AT 13:48I hear you, but let’s not forget the human side of this. A patient dealing with chronic kidney disease can’t afford to gamble with a drug that might add stones to their list of worries. Empathy matters – choosing a regimen that respects their health and lifestyle is essential. Even if the price is a bit higher, the peace of mind from fewer side effects can be priceless. Let’s keep compassion at the forefront of our prescribing decisions.
shikha chandel
October 11, 2025 AT 06:28Indinavir is antiquated, lacks elegance, and its pharmacodynamics are subpar.
Zach Westfall
October 11, 2025 AT 23:08Got to say the table is neat it lays everything out clear but i wish they added a column for drug‑drug interactions especially with common statins the side effect list is solid though i’d love more on the lipid profile changes you know what i mean?
Pranesh Kuppusamy
October 12, 2025 AT 15:48In the grand tapestry of antiretroviral therapy, each protease inhibitor occupies a niche defined not merely by its biochemical potency but by the socioeconomic realities of the patient. To privilege cost over tolerability is a false dichotomy; the true optimization lies in a holistic assessment of adherence potential, comorbidities, and health system infrastructure.
Crystal McLellan
October 13, 2025 AT 05:41They don’t tell you that the pharma giants are secretly embedding nano‑chips in the pills to track us. That's why the newer PIs seem so fancy – they’re part of the surveillance network. Stick with the old stuff, you know, the one they don’t push on social media. Stay woke.
Kelly Thomas
October 13, 2025 AT 19:34Hey folks, happy to help! When weighing Indinavir against the newer protease inhibitors, think about three core pillars: efficacy, tolerability, and adherence. First, efficacy – all of the agents listed achieve comparable viral suppression when combined with a solid backbone regimen, so you’re not losing ground by choosing a newer PI. Second, tolerability – Indinavir’s propensity for kidney stones and hyperbilirubinemia can be a real hurdle; atazanavir’s mild indirect hyperbilirubinemia is usually asymptomatic, while darunavir’s diarrhea can be managed with diet and hydration. Third, adherence – once‑daily dosing (atazanavir, darunavir) dramatically improves pill‑burden, which studies show translates into higher long‑term viral control. Cost is another factor; while the generic price of Indinavir hovers around $1,200 per month, remember that hidden expenses like kidney‑function monitoring and potential stone‑related interventions can offset any savings. In contrast, the newer agents, even if slightly pricier, often come with patient‑assistance programs that shrink out‑of‑pocket costs. Bottom line: for patients with stable renal function and no adherence concerns, Indinavir remains a viable, cost‑effective choice. For anyone dealing with kidney issues, a high‑fat‑meal requirement, or who struggles with twice‑daily dosing, the modern once‑daily options are usually the smarter route. Feel free to ping me if you need deeper dive into drug–drug interaction charts or assistance navigating insurance formularies!
Mary Ellen Grace
October 14, 2025 AT 09:28Thanks for the info! I think the table is super helpful and the quick summary nails the main points. It’s nice to see a clear breakdown – makes it easier to decide which med might work best for me.
Carl Watts
October 14, 2025 AT 23:21The evolution of protease inhibitors mirrors the philosophical journey from mechanistic reductionism to a more holistic understanding of patient-centered care. We must ask not only which molecule achieves the lowest viral load, but also which regimen harmonizes with the lived experience of the individual, respecting their daily rhythms, cultural practices, and economic constraints. In this sense, the choice of indinavir versus atazanavir becomes a micro‑cosm of the broader ethical deliberations that define modern medicine.
Brandon Leach
October 15, 2025 AT 13:14Ah yes, because the world needed another once‑daily pill to solve all our problems. Brilliant, really.
Alison Poteracke
October 16, 2025 AT 00:21Hi all! Just a quick friendly reminder: when picking a PI, think about your daily routine. If you travel a lot or have erratic meal times, a drug that doesn’t need food (like darunavir) might be best. And don’t forget to ask your pharmacist about any discount cards – they can shave a lot off the price.
Marianne Wilson
October 16, 2025 AT 11:28Honestly, the whole "newer is better" narrative is just a marketing ploy. People forget that the old drugs have stood the test of time, and swinging to the latest version just because it sounds shinier is ethically dubious. If you’re not convinced by solid data, you’re being swayed by hype.
Patricia Bokern
October 16, 2025 AT 22:34OMG, can we talk about how dramatic the kidney stone thing is? Like, seriously, who wants to deal with that? It’s like a horror movie every time you have to pee! 🙀
Garrett Gonzales
October 17, 2025 AT 09:41From a pharmacoeconomic perspective, the incremental cost‑effectiveness ratio (ICER) of atazanavir versus indinavir favors the former when you factor in quality‑adjusted life years (QALYs) lost due to renal complications. The once‑daily dosing also reduces indirect costs associated with non‑adherence, which can be quantified using the medication possession ratio (MPR) metric. In short, newer PIs provide a better value proposition in most health system models.
Aman Deep
October 17, 2025 AT 18:01🌈 Wow, what a colorful spectrum of options! From the gritty, stone‑prone indinavir to the sleek, once‑daily wonders, it’s like choosing between a vintage vinyl and a streaming playlist. 🎶 Just remember, the best track is the one that keeps you dancing to life’s rhythm, not the one that makes you miss a beat because of side effects. 🎵
Herman Bambang Suherman
October 18, 2025 AT 02:21Choosing a PI should align with your health goals and daily schedule; consider adherence, side‑effect profile, and cost. A concise, balanced approach works best.