When you're on antibiotics, your body is fighting an infection-but it's also wiping out good bacteria along the way. That’s where probiotics come in. But if you take them at the wrong time, they might not work at all. Probiotics and antibiotics don’t mix well when taken together without spacing. The antibiotics kill the good bugs before they even have a chance to settle in. The good news? A simple 2-hour gap can make all the difference.
Why Timing Matters
Antibiotics don’t pick and choose. They go after bacteria-both the bad ones causing your infection and the good ones living in your gut. This disruption can lead to diarrhea, bloating, yeast overgrowth, or even a serious infection like C. diff. About 30% of people on antibiotics experience these side effects. Probiotics help, but only if they survive long enough to do their job. Research shows that if you take probiotics at the same time as your antibiotic, up to 92% of the good bacteria die before they can colonize. That’s not just ineffective-it’s a waste of money. But when spaced properly, probiotics can cut your risk of antibiotic-associated diarrhea by nearly half.The 2-Hour Rule
The gold standard is simple: take your probiotic at least two hours before or after your antibiotic dose. This isn’t arbitrary. Antibiotics are absorbed and cleared from your gut within about 90 minutes to 2 hours. Waiting two hours gives them time to leave your system before the probiotics arrive. For example, if you take amoxicillin at 8 a.m. and 8 p.m., your probiotic should be taken at 6 a.m. and 6 p.m., or 10 a.m. and 10 p.m. That keeps a clean buffer. Some doctors even suggest 4 to 6 hours for stronger antibiotics like clindamycin or ciprofloxacin, especially if you’ve had gut issues before.Which Probiotics Work Best?
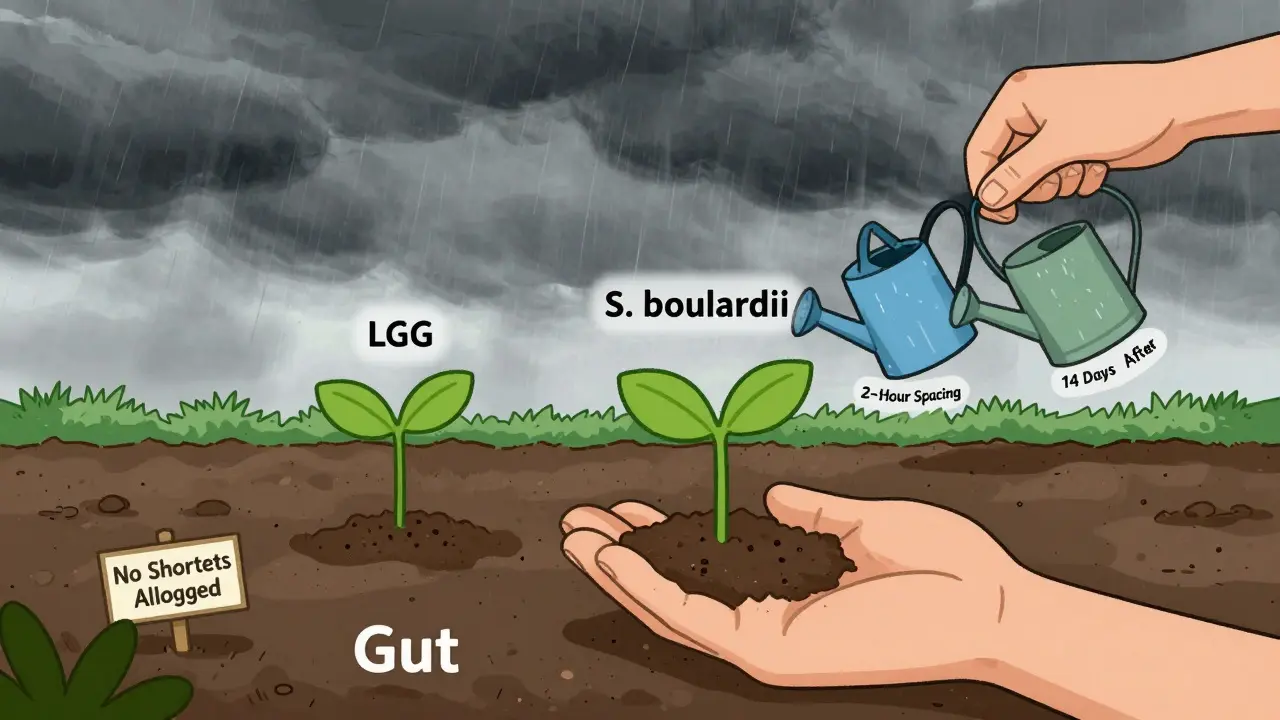
Not all probiotics are created equal. The strain matters more than the number of billions. Here’s what the science says:- Lactobacillus rhamnosus GG (LGG): Proven to reduce diarrhea risk by 47%. Best at 10-20 billion CFU per day.
- Saccharomyces boulardii: A yeast, not a bacteria. It’s immune to most antibiotics, so you can take it with your dose. Reduces diarrhea risk by 52% at 20 billion CFU.
- Bifidobacterium species: Helpful for long-term recovery, especially after extended antibiotic use.
Multi-strain products? They sound better, but studies show they’re not significantly more effective than single-strain options. Stick with strains that have real data behind them.
How Long Should You Keep Taking Them?
Don’t stop when the antibiotics run out. Your gut needs time to rebuild. Experts recommend continuing probiotics for 7 to 14 days after your last antibiotic dose. Some studies show people who stuck with it for 14 days had 89% better microbiome recovery than those who quit early. Think of it like planting a garden after a storm. You don’t just sow seeds and walk away. You water them, protect them, and give them time to grow. Your gut is the same.
What About Yeast vs. Bacteria?
This is a key detail many people miss. Most probiotics are bacteria, and they’re vulnerable to antibiotics. But Saccharomyces boulardii is a yeast. It doesn’t care about antibiotics. So if you’re using this one, you can take it at the same time as your antibiotic without losing effectiveness. That’s a game-changer for people who forget to space out doses. If you’re using LGG or another bacterial strain, stick to the 2-hour rule. If you’re using S. boulardii, you can take it with your pill-no waiting needed.What If You Forget to Space Them?
Life happens. You’re running late, you’re tired, or you just forgot. Missing one dose won’t ruin everything, but consistency matters. Studies show skipping probiotic doses reduces effectiveness by 37%. If you accidentally take them together, don’t panic. Just wait until the next scheduled dose and space them properly from then on. The real problem isn’t occasional mistakes-it’s chronic inconsistency. People who stick to the schedule have far better outcomes. Set phone alarms. Keep your probiotic next to your antibiotic bottle. Make it part of your routine.What to Look for on the Label
Here’s the ugly truth: only 32% of probiotic products on the market list the exact strain. Without knowing the strain, you can’t know if it’s backed by science. Look for these names on the label:- Lactobacillus rhamnosus GG
- Saccharomyces boulardii CNCM I-745
- Bifidobacterium animalis subsp. lactis BB-12
These strains have been tested in clinical trials. Avoid products that just say “proprietary blend” or “10 billion CFU” without naming the strains. You’re guessing.
When to Be Cautious
Most people benefit from probiotics during and after antibiotics. But if you’re immunocompromised, have a central line, or have severe gut damage, talk to your doctor first. In rare cases, probiotics can cause infections in vulnerable people. Also, some newer research suggests that for certain broad-spectrum antibiotics-like those that wipe out a huge chunk of your microbiome-waiting until after treatment to start probiotics might help your gut recover more naturally. But this is still being studied. For now, the standard advice still holds: start early, space them, keep going.What’s Changing in the Future
Companies are working on time-release capsules and acid-resistant coatings that might let probiotics survive even when taken with antibiotics. Some are even testing combo pills that release the antibiotic first, then the probiotic hours later. But none of these are available yet. For now, the 2-hour rule is still the most reliable, evidence-backed method. It’s simple, cheap, and backed by over 20 years of research across 31 major medical institutions.Final Checklist
- Choose a probiotic with a proven strain: LGG or S. boulardii.
- Take 20-40 billion CFU per day, depending on how long you’re on antibiotics.
- Space probiotics at least 2 hours apart from antibiotics.
- Keep taking probiotics for 7-14 days after your last antibiotic dose.
- If using S. boulardii, you can take it with the antibiotic.
- Set reminders. Don’t rely on memory.
Antibiotics save lives. Probiotics help your body recover. But they only work if you give them a fighting chance. A two-hour gap isn’t a suggestion-it’s the difference between a gut that bounces back and one that stays out of balance for months.
Can I take probiotics at the same time as antibiotics?
Only if you're using a yeast-based probiotic like Saccharomyces boulardii. It’s not affected by antibiotics. For bacterial probiotics like Lactobacillus or Bifidobacterium, taking them at the same time kills up to 92% of the live bacteria. Always space bacterial probiotics at least two hours apart from antibiotics.
How many CFUs should I take?
For most people on a short course (3-5 days), 5-10 billion CFU is enough. If you’ve had diarrhea before or are on antibiotics for more than a week, go with 10-20 billion CFU. For long courses (over 14 days) or if you have existing gut issues, 20-40 billion CFU is recommended. Always check the strain-dose matters less than the right bacteria.
Do I need a multi-strain probiotic?
No. Studies show multi-strain products aren’t more effective than single-strain ones for preventing antibiotic-associated diarrhea. In fact, some just cost more. Stick to strains with strong evidence: Lactobacillus rhamnosus GG or Saccharomyces boulardii. More strains don’t mean better results.
How long should I keep taking probiotics after antibiotics?
Continue for 7 to 14 days after your last antibiotic dose. This gives your gut time to rebuild its natural balance. One study found people who took probiotics for 14 days after antibiotics had 89% better microbiome recovery than those who stopped earlier. Don’t stop just because you feel better.
What if I accidentally take them together?
Don’t panic. One mistake won’t ruin everything. Just go back to spacing them 2 hours apart for the next dose. Consistency over time matters more than perfection. If you miss a day, take the next one as scheduled. The goal is daily adherence, not flawless timing every single time.
Are all probiotics the same?
No. Only about 32% of probiotic products list the exact strain. Without knowing the strain, you can’t be sure it’s effective. Look for names like Lactobacillus rhamnosus GG or Saccharomyces boulardii CNCM I-745. Avoid products that say "proprietary blend" or only list CFUs without strain names.
Can probiotics delay gut recovery?
Some new research suggests that in rare cases, certain probiotics might slow natural recovery after broad-spectrum antibiotics. But this is still being studied. For most people, the benefits of reducing diarrhea and preventing C. diff far outweigh this potential risk. Stick with proven strains and follow spacing guidelines unless your doctor advises otherwise.
If you're on antibiotics right now, your gut is under stress. Probiotics can help-but only if you give them the right conditions. Two hours apart. Daily. For two weeks after. That’s the recipe.






Jonah Mann
February 8, 2026 AT 22:14THANGAVEL PARASAKTHI
February 10, 2026 AT 18:34Brandon Osborne
February 11, 2026 AT 03:49Tatiana Barbosa
February 11, 2026 AT 19:23Ken Cooper
February 12, 2026 AT 21:23MANI V
February 13, 2026 AT 02:47Susan Kwan
February 13, 2026 AT 14:36Random Guy
February 14, 2026 AT 14:03Ryan Vargas
February 14, 2026 AT 21:29Tasha Lake
February 15, 2026 AT 12:23Sam Dickison
February 15, 2026 AT 13:46Jacob den Hollander
February 17, 2026 AT 00:50Andrew Jackson
February 17, 2026 AT 20:23