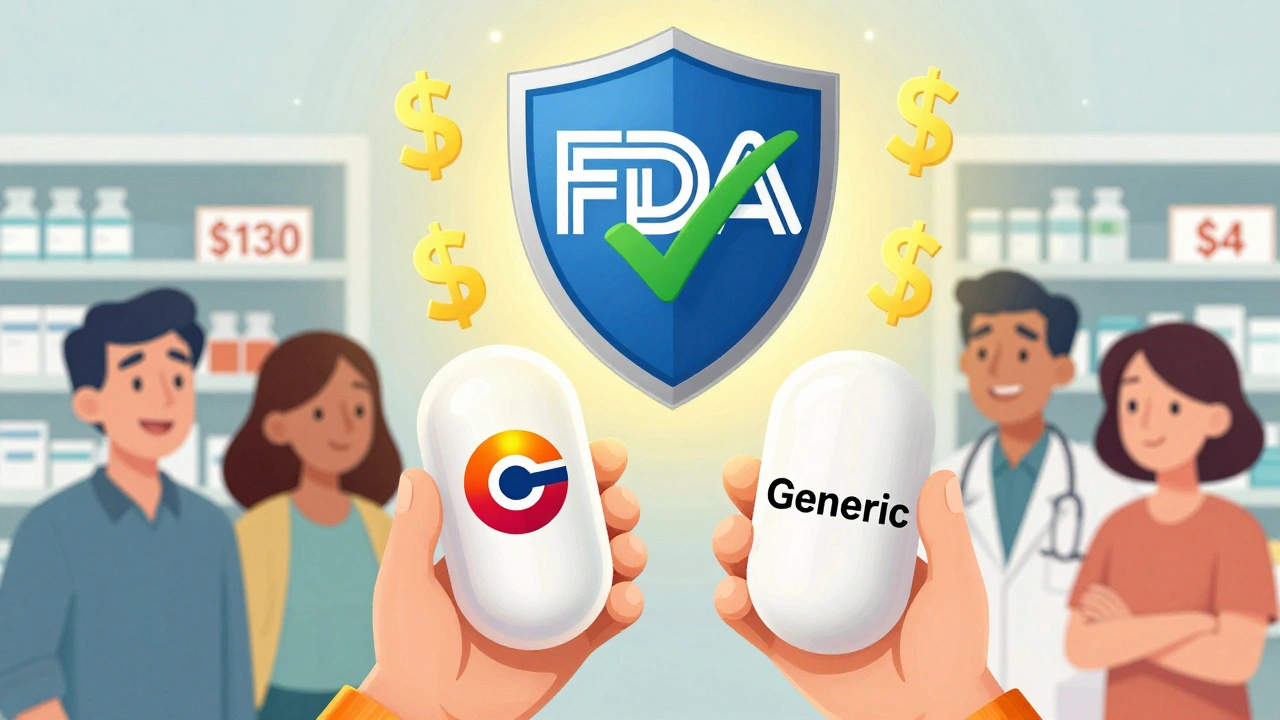
Every year, millions of people in the U.S. and around the world face a simple but painful choice: pay hundreds of dollars for a brand-name pill, or switch to a generic version that costs a fraction of the price. If you’ve ever wondered whether the cheaper option is really the same, you’re not alone. The truth? Generic medications aren’t just cheaper-they’re just as safe and effective as the brand-name versions you’ve been told to trust.
They’re the Same Drug, Just Without the Brand Name
Let’s clear up the biggest myth right away: a generic drug isn’t a copy, a knockoff, or a lower-quality substitute. It’s the exact same medicine. The active ingredient-the part that actually treats your condition-is identical. If your doctor prescribed atorvastatin for high cholesterol, the generic version is still atorvastatin. Same molecule. Same effect. Same science.
The U.S. Food and Drug Administration (FDA) requires generics to meet the same strict standards as brand-name drugs. That means the same strength, the same dosage form (pill, liquid, injection), the same way it’s absorbed into your body, and the same intended use. The only differences? The color, shape, or inactive ingredients like fillers or dyes. These don’t affect how the drug works. They’re just there to make the pill look different or easier to swallow.
Cost Savings Are Real-Sometimes Life-Changing
Here’s where it gets powerful. Generic drugs cost, on average, 80% to 85% less than their brand-name counterparts. That’s not a small discount. That’s a revolution in access.
Take Lipitor, the brand-name cholesterol drug. Before its patent expired, it cost around $130 a month. Today, the generic version, atorvastatin, costs as little as $4 at major pharmacies. Warfarin, a blood thinner, used to be sold as Coumadin for over $300 a month. Now, the generic runs about $4 for a 30-day supply. For someone on a fixed income, that’s not just savings-it’s the difference between taking your medicine and skipping doses.
Across the board, the numbers speak for themselves. In 2023, generics made up 90% of all prescriptions filled in the U.S., but only 23% of total drug spending. That means 9 out of 10 pills you pick up are generic, and they’re saving the system over $1.6 trillion in the last decade alone. For individual patients, switching means lower copays. Most insurance plans charge $1-$10 for generics versus $25-$75 for brand-name drugs. For Medicare Part D beneficiaries, the average cost per generic prescription is just $1.85. For brand-name? Over $33.
They Work Just as Well-Here’s the Proof
Some people worry: if it’s cheaper, does it work as well? The answer is yes-over and over again.
A 2022 study in the Journal of Managed Care & Specialty Pharmacy looked at thousands of patients taking generic versus brand-name heart medications for high blood pressure and heart failure. No difference in outcomes. No increase in hospital visits. No drop in effectiveness.
Another large study in the Journal of the American Heart Association followed 186,000 patients on generic versus brand-name heart drugs. The results? Identical rates of heart attacks, strokes, and deaths. Dr. Aaron Kesselheim from Harvard Medical School, who led the research, said: “Our research confirms that generic cardiovascular drugs perform as well as their brand-name counterparts.”
The FDA doesn’t approve generics unless they’re bioequivalent-meaning they deliver the same amount of active ingredient into your bloodstream at the same rate as the brand-name drug. The standard? The concentration in your blood has to fall within 80% to 125% of the brand-name version. That’s not a wide gap. It’s tight. It’s science.

What About Those Rare Cases?
There’s one group of drugs where people sometimes raise concerns: narrow therapeutic index (NTI) drugs. These are medications where even a tiny change in blood levels can affect how well they work-or cause side effects. Examples include warfarin, some epilepsy drugs like phenytoin, and thyroid meds like levothyroxine.
Even here, the FDA says approved generics meet the same standards. But some doctors, like neurologists at the Mayo Clinic, suggest that for certain patients on NTI drugs, switching between different generic manufacturers might cause subtle changes in how they feel. That’s not because the drug is inferior. It’s because every person’s body reacts differently, and switching pill shapes or fillers can sometimes trigger anxiety or minor side effects.
The fix? Stick with the same generic manufacturer once you’ve found one that works. If your pharmacy switches the brand of generic you’re on, ask them to let you know. You can request the same version. Most pharmacists will honor that.
Real People, Real Savings
Stories from patients tell the real story.
One Reddit user, PharmTech87, wrote: “Switching my blood pressure meds to generic saved me $280 a month-no side effects, no drop in control.”
A diabetes patient on PatientsLikeMe shared: “Metformin generics cost me $4 a month. Glucophage (the brand) was $300. This keeps me alive.”
Kaiser Permanente’s 2023 survey showed 87% of patients were satisfied with generics. The top reason? Affordability. Only 3% reported any issue with effectiveness.
And here’s the kicker: people who use generics are 68% less likely to skip doses because they can’t afford them. That’s not just about money. It’s about health. It’s about living longer.
How to Switch-And What to Expect
Switching is easy. Your doctor can prescribe the generic version from the start. Or, when your prescription runs out, your pharmacist may automatically substitute it-unless you say no. In most states, pharmacists are allowed to switch to a generic unless the doctor writes “Dispense as Written” or “Do Not Substitute.”
When you get your new prescription, check the pill. It might look different. That’s normal. The shape, color, or imprint might change. That doesn’t mean it’s not the same drug. Ask your pharmacist to show you the label and confirm the active ingredient matches what your doctor prescribed.
If you’re nervous, bring up the FDA’s “Generic Drug Facts” page during your next visit. Print it out. Show it to your doctor. Most will be happy to explain it to you.

Why Don’t More People Switch?
It’s not about science. It’s about perception. Many people believe “brand-name = better.” That’s marketing, not medicine. It’s also fear. Changing the look of a pill can trigger anxiety. “Is this the right one?” “Did they mess up?”
But here’s what you need to remember: your body doesn’t care about the logo on the pill. It cares about the chemical inside. And that chemical? It’s the same.
Pharmacies and insurers push generics because they save money. But they also push them because they know they work. Hospitals use them. The VA uses them. Medicare uses them. If they weren’t safe and effective, they wouldn’t be the standard.
What’s Next? Biosimilars and Beyond
The next wave is biosimilars-generic versions of complex biologic drugs like Humira or Enbrel. These aren’t simple pills. They’re made from living cells. But the same rules apply: they must match the original drug in safety and effectiveness. As of 2023, the FDA has approved 37 biosimilars. Experts predict they’ll save Medicare $50 billion a year by 2030.
And the FDA is working harder than ever to get more generics on the market faster. Their 2023 Drug Competition Action Plan targets barriers that delay generic entry-especially for inhalers, eye drops, and topical creams. The goal? More choices. Lower prices. Better access.
Bottom Line: Switching Makes Sense
Generic medications are not a compromise. They’re a smart, proven, and safe choice. They save you money. They save the system money. And they work just as well as the brand-name drugs you’ve been paying more for.
If you’re on a brand-name drug and not sure whether a generic is available, ask your pharmacist or doctor. Check your insurance formulary. Look up your medication on the FDA’s Orange Book. You might be surprised at how much you could save-without losing a single bit of effectiveness.
There’s no reason to overpay for the same medicine. The science is clear. The savings are real. And your health? It stays exactly the same.
Are generic medications as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict standards for safety, strength, quality, and performance as brand-name drugs. They must prove bioequivalence-meaning they deliver the same amount of active ingredient into your bloodstream at the same rate. Adverse event reports for generics are proportional to how often they’re used, showing no higher risk than brand-name drugs.
Why do generic pills look different?
Generic pills can look different because U.S. law requires them to have a different appearance than the brand-name version to avoid trademark infringement. This includes color, shape, size, or markings. These changes are only cosmetic. The active ingredient, dosage, and effectiveness remain identical. If you’re concerned, ask your pharmacist to confirm the active ingredient matches your prescription.
Can I switch back to the brand-name drug if I don’t like the generic?
Yes. If you feel the generic isn’t working the same way-or if you’re anxious about the change-talk to your doctor. They can write a prescription that says “Dispense as Written” or “No Substitution.” However, your insurance may charge a higher copay, and you’ll pay more out of pocket. Most people find no difference, but your comfort matters too.
Do generics take longer to work?
No. The FDA requires generics to be bioequivalent, meaning they enter your bloodstream at the same rate and to the same extent as the brand-name version. There’s no delay in how quickly they start working. If you feel a difference in timing, it’s likely due to psychological factors or changes in inactive ingredients-not the active drug.
Are all generic drugs made in the U.S.?
No. Many generic drugs are manufactured in countries like India and China. But the FDA inspects all manufacturing facilities-domestic and international-before approving a generic. In 2023, the FDA conducted over 1,200 inspections worldwide. The same quality standards apply regardless of where the drug is made. The FDA doesn’t allow lower-quality imports.
Why do generic prices vary so much between pharmacies?
Generic prices vary because multiple manufacturers produce the same drug, and competition drives prices down. Some pharmacies offer discounts through cash programs (like Walmart’s $4 list), while others rely on insurance contracts. Always compare prices. Use tools like GoodRx or your pharmacy’s app to find the lowest cost. Sometimes the same generic costs $3 at one pharmacy and $15 at another.
Is it safe to switch between different generic brands?
For most medications, yes. But for drugs with a narrow therapeutic index-like warfarin, thyroid meds, or some seizure drugs-switching between generic manufacturers can sometimes cause small changes in how your body responds. If you’re on one of these, ask your pharmacist to stick with the same manufacturer. If you notice new side effects after switching, contact your doctor.




Desmond Khoo
December 7, 2025 AT 03:28Just switched my blood pressure med to generic last month and my wallet cried happy tears 😭 $4 vs $280? No contest. My BP’s stable, no weird side effects, and I’m finally saving enough to take that trip I’ve been putting off. Life’s good when science and savings align.
Wesley Phillips
December 9, 2025 AT 00:19Look I get it generics are cheaper but come on you’re telling me a pill made in India with fillers I can’t pronounce is the same as the one my cardiologist prescribed? I’ve seen too many horror stories on the news. This isn’t just about money it’s about trust.
Olivia Hand
December 10, 2025 AT 04:08Interesting. I’ve been on generic levothyroxine for 5 years but my pharmacy switched manufacturers last month and I felt… off. Not bad just… different. My endo said it’s common with NTI drugs and I should stick with the same brand. Never thought the color of the pill could mess with my energy levels.
Louis Llaine
December 11, 2025 AT 22:26Oh wow so the government says it’s fine. That’s reassuring. Next you’ll tell me my iPhone charger from Alibaba is just as good as the Apple one. At least the brand-name one didn’t melt my outlet.
Kurt Russell
December 12, 2025 AT 00:14STOP OVERPAYING. Seriously. I used to spend $150/month on my diabetes meds. Now I pay $5. I’m alive. I’m healthy. I’m not broke. This isn’t a gamble. This is common sense. If your doctor won’t prescribe it ask for a second opinion. Your future self will thank you.
Stacy here
December 12, 2025 AT 23:23Did you know the FDA approves generics using data from the brand-name companies? That’s right. The same lab that made Lipitor also tested the generic. Who’s really controlling the narrative here? Big Pharma wants you scared of the blue pill. They don’t want you to know you’ve been paying for a logo.
Kyle Flores
December 13, 2025 AT 19:59Hey I get why people are nervous. I was too. My grandma switched to generic warfarin and panicked every time the pill looked different. We called the pharmacy and asked for the same manufacturer. She’s been fine for 3 years now. It’s okay to be cautious. Just don’t let fear cost you your health.
Ryan Sullivan
December 15, 2025 AT 18:13Let’s be clear. The FDA’s bioequivalence standard of 80–125% is a regulatory loophole masquerading as scientific rigor. A 25% variance in plasma concentration is not trivial. It’s a pharmacokinetic wild west. And yet we’re expected to treat this as equivalent? That’s not medicine. That’s statistical gymnastics dressed in white coats.
When I see a patient on a generic with fluctuating INRs or erratic seizure control, I don’t blame them. I blame the system that reduced therapeutic certainty to a confidence interval.
Don’t get me wrong - generics have their place. But to pretend they’re interchangeable without oversight is irresponsible. The data is there. The outliers are real. And the cost savings come at the expense of clinical nuance.
David Brooks
December 16, 2025 AT 13:00THIS. This is the kind of post that saves lives. I was on $300/month for my heart med until I switched. Now I pay $4. I’m not just surviving - I’m playing guitar again. I’m hiking with my grandkids. Don’t let fear or marketing steal your health. Ask your pharmacist. Ask your doctor. Just DO IT.
Nicholas Heer
December 17, 2025 AT 06:19Generics made in CHINA? Yeah right. You think the FDA inspects every factory? They got more inspections than a DMV line. Half those pills are shipped in unmarked crates. And now you want me to swallow them? My grandfather fought in WWII so we could be free from foreign control. Now we’re swallowing pills made by people who don’t even speak English. This isn’t healthcare. It’s national surrender.
Sangram Lavte
December 18, 2025 AT 11:30Used to work in a pharmacy in Mumbai. We shipped generic metformin to the US every week. The same batch that went to India went to Chicago. Same factory. Same machine. Same quality. If you trust your insulin, trust your metformin. Money matters but so does truth.
Jane Quitain
December 19, 2025 AT 22:17Just switched to generic and my anxiety went up because I kept checking if it was the right pill 😅 but after a week I forgot what the brand looked like and now I’m just saving money. Thank you for this post! I didn’t know generics were this legit.