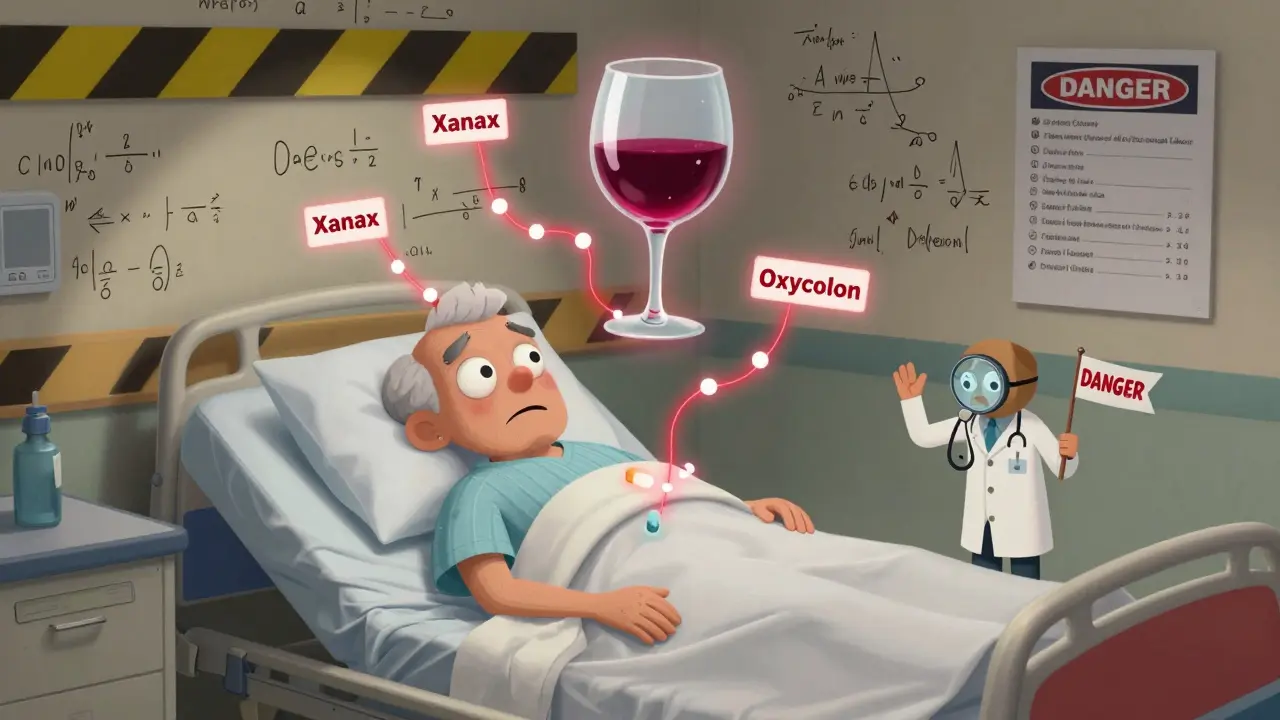
Many people don’t realize that drinking alcohol while taking medication can be just as dangerous as taking the wrong pill. It’s not just about feeling more tired or getting a bad hangover. In some cases, mixing alcohol and meds can land you in the hospital-or worse. The truth is, alcohol and medications don’t mix safely in most situations, and the risks are far higher than most people think.
How Alcohol Changes How Your Medicines Work
Alcohol doesn’t just sit there quietly in your body. It’s processed by your liver, the same place where most medications are broken down. When you drink, your liver gets busy dealing with alcohol first. That means your meds might not get processed the way they should. Sometimes they stick around too long. Other times, they break down into toxic substances your body wasn’t meant to handle. There are three main ways alcohol messes with your meds:- Pharmacokinetic interactions: Alcohol changes how your body absorbs, moves, or gets rid of the drug. For example, it can slow down how fast a painkiller leaves your system, making it build up to dangerous levels.
- Pharmacodynamic interactions: Alcohol and the drug both hit the same part of your brain or body, making their effects multiply. This is why mixing alcohol with sleep aids or painkillers can shut down your breathing.
- Toxic reactions: Some combinations create new chemicals inside your body that aren’t just harmful-they’re deadly. Acetaminophen (Tylenol) and alcohol is the most common example.
Deadly Combinations: The High-Risk Meds
Not all meds are equally dangerous with alcohol. But some combinations are life-threatening. Here’s what you need to know:Opioids: Painkillers + Alcohol = Breathing Failure
If you’re taking oxycodone, hydrocodone, morphine, or methadone, alcohol is a red flag. These drugs already slow your breathing. Alcohol does the same. Together, they can stop your breathing completely. The CDC found that 20% of opioid overdose deaths in 2020 involved alcohol. The FDA pulled a long-acting opioid called Palladone off the market in 2005 after studies showed alcohol caused a sudden, massive release of the drug-like a bomb going off inside your body.Benzodiazepines: Anxiety Pills + Alcohol = Unconsciousness
Drugs like Xanax, Valium, and Ativan are prescribed for anxiety and sleep. They’re CNS depressants. So is alcohol. Mix them, and your brain’s ability to control breathing and heart rate plummets. A 2019 study showed this combo increases overdose risk by 24 times. People don’t always realize they’re mixing them-many take a pill for anxiety and then have a glass of wine to relax. That’s not relaxation. That’s a gamble with your life.Acetaminophen: Tylenol + Alcohol = Liver Failure
This one catches people off guard because Tylenol is so common. Your liver turns acetaminophen into a toxic byproduct called NAPQI. Normally, your body neutralizes it with antioxidants. But alcohol drains those antioxidants. Now NAPQI builds up and starts killing liver cells. The FDA says acetaminophen overdoses-often caused by alcohol-lead to 56,000 ER visits, 26,000 hospital stays, and nearly 500 deaths every year in the U.S. Even one drink with a regular dose of Tylenol can push you into danger if you’re a regular drinker.Metronidazole: Antibiotic + Alcohol = Poisoning
If you’re on Flagyl for an infection, don’t touch alcohol. Not even a sip. It triggers a disulfiram-like reaction: nausea, vomiting, flushing, racing heart, chest pain. It’s not just uncomfortable-it can cause your blood pressure to crash. The Illinois Poison Center says you need to wait at least 72 hours after your last dose before drinking.Other Dangerous Mixes You Might Not Expect
Some interactions aren’t instantly deadly, but they’re still risky-and often ignored.- NSAIDs (Ibuprofen, Naproxen): These painkillers already irritate your stomach lining. Alcohol does too. Together, they can cause severe bleeding in your gut. Studies show the risk triples to five times higher.
- Antidepressants (SSRIs like Prozac, Zoloft): Alcohol makes depression worse. It also reduces how well the medication works. Plus, it can increase dizziness and drowsiness, raising fall risk-especially in older adults.
- Blood pressure meds: Alcohol can make your blood pressure drop too low, especially when standing up. This causes dizziness, fainting, and falls. The risk is highest in seniors.
- Diabetes meds (Sulfonylureas, Metformin): Alcohol can trigger dangerous low blood sugar. With sulfonylureas, the risk jumps 300%. With metformin, alcohol increases the chance of lactic acidosis, a rare but deadly buildup of acid in the blood.
- ADHD meds (Adderall, Ritalin): These are stimulants. Alcohol is a depressant. The clash masks how drunk you are, so you drink more. It also puts extra strain on your heart and can cause irregular heartbeat.
- Antihistamines (Benadryl, Zyrtec): Both cause drowsiness. Together, they can make you too sleepy to drive-or even stay awake.
Who’s at the Highest Risk?
It’s not just about what you take-it’s who you are.- People over 65: Your liver and kidneys don’t work as well. You’re more likely to be on five or more medications. The Beers Criteria lists 30 drugs that are especially risky for seniors when mixed with alcohol. One study found 82% of older adults take at least one med that could interact badly with alcohol.
- Women: Women have less water in their bodies than men. That means alcohol stays more concentrated. Same drink, higher blood alcohol level. That makes interactions more dangerous.
- People with mental health conditions: Those with depression, anxiety, or PTSD are more likely to use both alcohol and prescription meds. SAMHSA says this group has alcohol-medication interactions 3.5 times more often than others.
- Veterans: The VA found that 30% of veteran suicides involved alcohol and prescription drugs. Many are on opioids, benzodiazepines, or antidepressants-and use alcohol to cope.
What You Should Do
You don’t need to give up alcohol entirely. But you need to be smart.- Read the label. The FDA requires alcohol warnings on about 100 prescription drugs and 700 over-the-counter meds. If it says “avoid alcohol,” don’t ignore it.
- Ask your pharmacist. They’re trained to spot these interactions. When you pick up a new prescription, ask: “Can I drink while taking this?”
- Know your meds. If you’re on multiple drugs, write them down. Bring the list to every doctor visit. Ask: “Which of these can’t I mix with alcohol?”
- Wait it out. If you’ve been on metronidazole, wait 72 hours after your last dose. For some meds, even 24 hours isn’t enough. When in doubt, skip it.
- Screen yourself. The NIAAA recommends the AUDIT-C test: three simple questions about how often and how much you drink. It’s used in clinics because it works.

The Bigger Picture
Doctors and pharmacists aren’t always asking about alcohol use. A 2022 study in JAMA Internal Medicine found only 35% of primary care doctors routinely ask patients about drinking when prescribing meds. That’s a gap. But you can fill it. New tech is helping. Electronic health systems like Epic now block doctors from prescribing high-risk meds if alcohol use is flagged. The FDA now requires new extended-release opioids to be tested for alcohol interactions before they’re approved. And research is moving toward genetic testing-some people have a version of the CYP2E1 enzyme that makes them 4.7 times more likely to suffer liver damage from acetaminophen and alcohol. Public health campaigns like the CDC’s “Alcohol and Medicine Don’t Mix” are trying to raise awareness. But real change happens one conversation at a time.Bottom Line
Alcohol isn’t just a social drink. It’s a powerful chemical that interacts with your body’s systems in ways you can’t always predict. When you add medication into the mix, the risks multiply. Some combinations are deadly. Others quietly damage your liver, stomach, or brain over time. You don’t have to be an expert to protect yourself. Just be curious. Ask questions. Read labels. Talk to your pharmacist. If a med says “avoid alcohol,” take it seriously. Your life might depend on it.Can I have one drink with my prescription meds?
It depends on the medication. For some, like blood pressure pills or antidepressants, one drink might be okay if you’re healthy and don’t drink often. But for others-like opioids, benzodiazepines, metronidazole, or acetaminophen-even one drink can be dangerous. There’s no universal safe amount. Always check with your doctor or pharmacist.
What if I forgot and had alcohol with my medicine?
If you took a small amount and feel fine, monitor yourself. Watch for dizziness, nausea, rapid heartbeat, confusion, or trouble breathing. If you’re on a high-risk med like an opioid or metronidazole and you feel unwell, seek medical help immediately. Don’t wait. Call poison control or go to the ER.
Are herbal supplements safe with alcohol?
No. Many herbal products aren’t tested for interactions. St. John’s Wort, kava, valerian, and echinacea can all affect your liver or nervous system. Mixing them with alcohol can increase sedation, raise liver damage risk, or cause unpredictable side effects. Treat them like regular meds-ask your pharmacist before combining.
Do over-the-counter meds have alcohol warnings too?
Yes. About 700 OTC products carry alcohol interaction warnings. This includes cold medicines, sleep aids, pain relievers, and antihistamines. Always read the “Drug Facts” label. Look for phrases like “do not use with alcohol” or “may cause drowsiness.”
Why do older adults face more risk?
As we age, our liver and kidneys process alcohol and drugs more slowly. We also tend to take more medications-sometimes 10 or more a day. This increases the chance of overlapping interactions. Plus, older adults are more sensitive to sedation, which raises fall and accident risk. The Beers Criteria specifically lists 30 drugs as unsafe for seniors when combined with alcohol.
Is it safe to drink the day before or after taking medication?
It depends on how long the drug stays in your system. For short-acting meds, 24 hours may be enough. For long-acting or extended-release drugs, it could be 48-72 hours. With metronidazole, you must wait 72 hours after the last dose. For acetaminophen, if you drink regularly, it’s safest to avoid it altogether. When unsure, wait longer.






Jhoantan Moreira
February 3, 2026 AT 02:16Amit Jain
February 4, 2026 AT 10:39rahulkumar maurya
February 4, 2026 AT 13:46Alec Stewart Stewart
February 5, 2026 AT 05:16Demetria Morris
February 6, 2026 AT 12:41Geri Rogers
February 8, 2026 AT 02:57Alex LaVey
February 10, 2026 AT 00:57caroline hernandez
February 10, 2026 AT 07:24Joseph Cooksey
February 11, 2026 AT 00:49Justin Fauth
February 12, 2026 AT 04:42Meenal Khurana
February 13, 2026 AT 00:57Joy Johnston
February 14, 2026 AT 19:50Shelby Price
February 16, 2026 AT 12:35Jesse Naidoo
February 16, 2026 AT 19:47Jhoantan Moreira
February 17, 2026 AT 11:31