When someone stops drinking after years of heavy alcohol use, their body doesn’t just feel shaky-it’s in a full-blown crisis. The liver, which has been working overtime to break down alcohol, suddenly has to shift gears. And that shift can be dangerous. Alcohol withdrawal isn’t just about anxiety or sweating. It’s a medical event that can damage the liver even after you’ve stopped drinking. Many people think quitting alcohol automatically means healing begins. But without the right approach, the liver can get worse before it gets better.
What Happens to Your Liver When You Stop Drinking?
Your liver processes 90% of the alcohol you consume. It turns ethanol into acetaldehyde-a toxic byproduct-then into acetate, which is harmless. But when you’ve been drinking heavily for months or years, your liver gets overwhelmed. Fat builds up. Inflammation sets in. Scar tissue starts forming. This is called alcohol-related liver disease (ALD), and it ranges from fatty liver to alcoholic hepatitis to cirrhosis.
When you stop drinking, the liver doesn’t magically fix itself. In fact, the first few days after quitting can be the most stressful for it. Blood flow to the liver changes. Metabolic pathways go haywire. And here’s the shocking part: liver enzyme levels often spike in the first week of withdrawal. A 2002 study found that 32% of heavy drinkers saw their AST and ALT (liver enzymes) rise sharply within 7 days of quitting. That doesn’t mean the liver is failing-it means it’s reacting to the sudden absence of alcohol and the body’s attempt to reset.
One key sign of alcohol-related liver damage is an AST:ALT ratio greater than 2:1. Normal ratios are below 1:1. If you’ve been drinking for years, your AST is likely much higher than your ALT. That’s a red flag. Other warning signs? Albumin below 3.5 g/dL or an INR (clotting time) over 1.5. These mean your liver is struggling to make proteins and manage blood clotting. At this point, home detox is risky.
The Real Danger: Paracetamol and Other Hidden Toxins
One of the most overlooked dangers during alcohol withdrawal is taking common painkillers like paracetamol (acetaminophen). You might think, “I have a headache-I’ll just take one tablet.” But your liver is in a fragile state. It’s already overloaded with detox work. And paracetamol? It’s processed by the same liver enzymes that handle alcohol.
Research from a 2002 study showed that even a small dose-1 to 2 grams of paracetamol per day-caused the biggest spike in liver enzymes among participants who had just stopped drinking. That’s less than the daily maximum dose recommended on the bottle. For someone with alcohol-related liver damage, this can trigger acute liver injury. And it can happen fast.
Other medications to avoid? NSAIDs like ibuprofen, certain antibiotics, and even some herbal supplements. Your liver doesn’t need extra stress right now. If you’re in withdrawal, don’t self-medicate. Talk to a doctor. If you need pain relief, ask what’s safe.
Medical Detox: Why It’s Not Optional for Most People
Unsupervised detox at home might sound cheaper and easier. But it’s not safer. A 2022 meta-analysis found that medically supervised detox has a 95% safety rate. Unsupervised detox? Only 65%. That’s a huge gap.
Why? Because withdrawal can spiral into delirium tremens (DTs)-a life-threatening condition with seizures, hallucinations, and extreme confusion. It affects about 5% of people with severe alcohol dependence. Without medical care, DTs can kill.
Doctors use benzodiazepines like chlordiazepoxide to prevent seizures and calm the nervous system. Chlordiazepoxide works in 85% of cases when given properly. Symptom-triggered protocols alone? Only 40% effective. That’s why hospitals and clinics don’t just monitor vital signs-they manage brain chemistry.
But here’s the catch: only 15% of rural communities in the U.S. have access to these facilities. That’s why telemedicine is helping. Since 2020, remote monitoring has expanded access by 25%. Still, if you have liver damage-elevated enzymes, low albumin, high INR-telemedicine alone isn’t enough. You need in-person care.
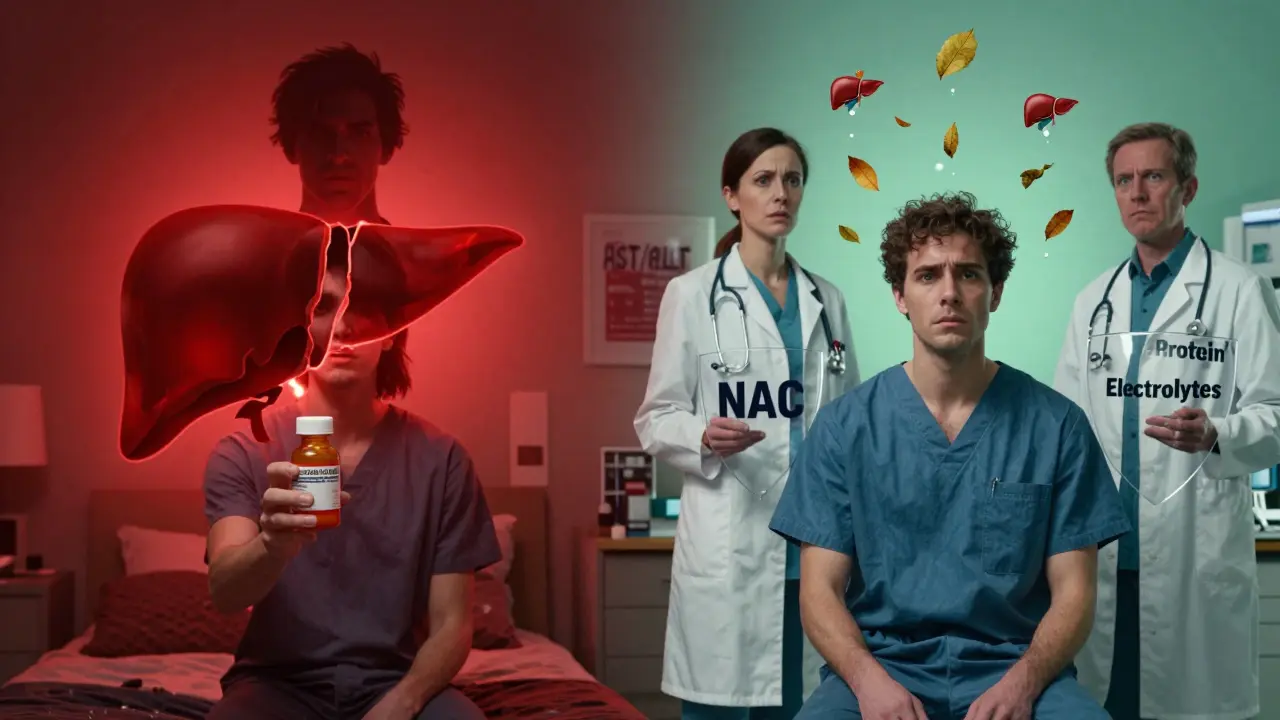
How to Support Your Liver During Detox
Detox isn’t just about stopping alcohol. It’s about giving your liver the tools to heal. Here’s what actually works:
- Thiamine (Vitamin B1): Give it IV daily for 3-5 days. Heavy drinkers are often severely deficient. Without it, you risk Wernicke-Korsakoff syndrome-a brain disorder that causes memory loss and confusion. This isn’t optional. It’s essential.
- Protein intake: Aim for 1.2 to 1.5 grams per kilogram of body weight. That’s about 80-100 grams daily for a 70kg person. Protein helps repair liver cells. Most detox programs skimp on this. Don’t.
- N-acetylcysteine (NAC): A 2021 trial showed NAC reduced liver enzyme spikes by 30% compared to placebo. It’s an antioxidant that helps your liver make glutathione, its main detox tool. Talk to your doctor about adding it.
- Hydration and electrolytes: Sweating, vomiting, and diarrhea during withdrawal drain your body. Replenish with water, broth, and oral rehydration solutions. Avoid sugary drinks-they worsen liver inflammation.
These aren’t “nice to have” tips. They’re medical necessities. A 2023 NHS guideline found that patients on this kind of support normalized liver enzymes 40% faster than those on standard care.
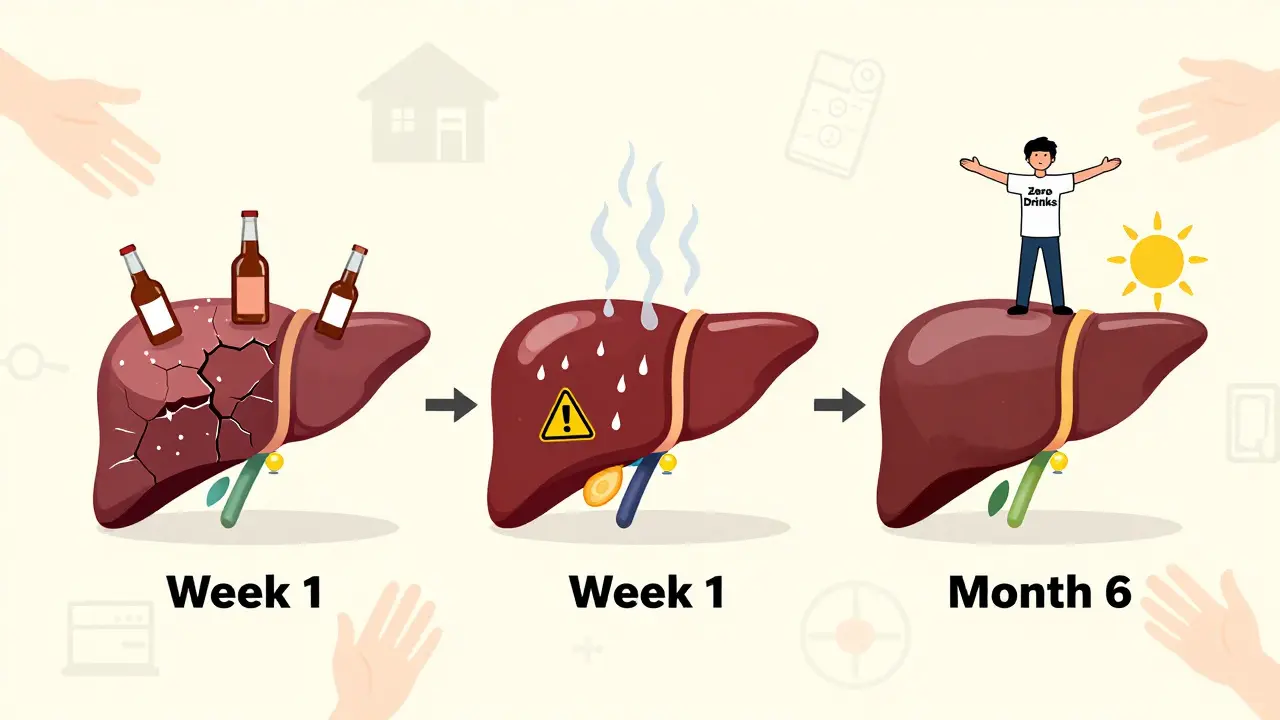
How Long Until Your Liver Heals?
Many people want to know: “How long until I’m back to normal?” The answer depends on how bad the damage was.
If you have fatty liver (early stage), stopping alcohol for 6 weeks can reverse it. That’s not a guess-it’s from clinical studies. Your liver can regenerate. It’s one of the few organs that can regrow damaged tissue.
But if you have alcoholic hepatitis or cirrhosis? You need lifelong abstinence. No exceptions. The Cleveland Clinic says it plainly: “If alcoholic hepatitis isn’t too far advanced, it can be reversed by quitting alcohol. Those who don’t quit will continue to progress toward cirrhosis and liver failure.”
Studies in Scientific Reports (2021) show that even after years of heavy drinking, liver function improves noticeably within 3-12 months of complete abstinence. Enzymes drop. Scarring slows. Blood flow improves. But this only happens if you don’t drink again.
And here’s a lesser-known fact: fibrosis can keep worsening during withdrawal. A 2020 study found that PIIINP-a marker of liver scarring-increases in the first weeks after quitting. That means your liver is still trying to repair itself, but the process is chaotic. That’s why ongoing medical monitoring matters.
What Not to Do After Detox
Detox is just the first step. The real challenge is staying stopped. And that’s where most people fail.
70% of those who complete detox relapse within 6 months if they don’t have ongoing support. That’s not weakness. It’s biology. Alcohol rewires your brain. Cravings are real. And if you start drinking again-even a little-you undo months of healing. One drink can restart inflammation. One binge can trigger liver failure.
Also, don’t assume “I only had a few drinks a day, so I’m fine.” The data shows that 40% of liver disease deaths in Western countries come from people who didn’t think they were “heavy” drinkers. It’s not about how much. It’s about how long.
And never go back to drinking “in moderation.” The NHS says if you had moderate to severe liver damage, even 14 units a week (the official UK limit) is too much. For you, zero is the only safe number.
When to Get Help
If you’re thinking about quitting, ask yourself:
- Have I been drinking heavily for more than 5 years?
- Do I have nausea, tremors, or anxiety when I haven’t had a drink?
- Have I ever passed out or had blackouts?
- Do I have high blood pressure, jaundice, or swelling in my legs?
If you answered yes to any of these, don’t try to quit alone. Go to a clinic. Call a helpline. Ask for a liver function test before you stop. If your enzymes are high, your body needs medical support.
And if you’ve already quit and are feeling worse-not better-get checked. A simple blood test can tell you if your liver is healing-or if it’s still in danger.
Can you reverse liver damage from alcohol?
Yes, but only if you stop drinking completely. Fatty liver can reverse in as little as 6 weeks. Alcoholic hepatitis can improve significantly within 3-6 months. But once cirrhosis sets in, the scarring is permanent. The liver can still function better if you stop drinking, but it won’t fully return to normal. The key is early action.
How long does alcohol withdrawal last?
Symptoms start 6-24 hours after the last drink. Peak symptoms happen in 2-3 days. Most physical symptoms fade in 5-7 days. But anxiety, sleep problems, and cravings can last weeks or months. The liver, however, takes longer to heal-weeks to months depending on damage. Medical supervision is critical in the first 72 hours.
Is it safe to detox from alcohol at home?
It’s risky. Only people with mild dependence and no liver damage should consider it-and even then, only with a doctor’s approval. If you’ve been drinking heavily for years, have high blood pressure, or have abnormal liver tests, home detox can lead to seizures, heart failure, or death. Medical detox reduces complications by 95% compared to unsupervised attempts.
Why is thiamine so important during alcohol withdrawal?
Chronic alcohol use depletes thiamine (vitamin B1), which your brain needs to function. Without it, you can develop Wernicke-Korsakoff syndrome-a condition that causes confusion, memory loss, and permanent brain damage. Giving thiamine IV during detox prevents this. It’s not optional. It’s life-saving.
Can I take painkillers like paracetamol after quitting alcohol?
Avoid it for at least the first 2 weeks. Your liver is extra sensitive during early withdrawal. Even small doses of paracetamol can cause severe liver injury. If you need pain relief, ask your doctor for alternatives like acetaminophen-free options or low-dose NSAIDs under supervision. Never self-prescribe.