Ever had a runny nose, stuffy nose, or sneezing that just won’t go away-but your allergy test came back negative? You’re not alone. For millions of people, especially those over 50, chronic nasal symptoms aren’t caused by pollen or pet dander. They’re caused by nonallergic rhinitis. Unlike allergic rhinitis, there’s no immune system overreaction. No IgE antibodies. No histamine flood. Just a nose that’s overly sensitive to things in the air, food, weather, or even your own medications.
What Exactly Is Nonallergic Rhinitis?
Nonallergic rhinitis is a chronic condition where your nasal passages react to irritants without any allergy involvement. It’s not infectious. It’s not autoimmune. It’s more like your nose has turned up the volume on every little environmental nudge. Symptoms include clear runny nose (rhinorrhea), nasal congestion, postnasal drip, and sneezing. These last for at least three months, and they don’t follow seasonal patterns like allergies do.It’s surprisingly common. Around 17-23% of adults in Western countries have it. That’s more than one in five people. And it gets worse with age. By the time you’re 70, up to 30% of people may be dealing with it. In fact, it’s the most frequent reason for chronic nasal symptoms in older adults-more than allergies.
Doctors diagnose it by ruling everything else out. Skin prick tests, blood tests for allergens, and nasal endoscopy are used to exclude allergies, infections, polyps, or structural issues. If all those come back normal and symptoms persist, it’s nonallergic rhinitis. The most common subtype? Vasomotor rhinitis. That’s when your autonomic nervous system-your body’s automatic control panel-gets confused. Too much parasympathetic activity means your nasal blood vessels swell and leak fluid. That’s the congestion and dripping.
The Top Irritant Triggers You Can’t Ignore
This is where it gets personal. Nonallergic rhinitis isn’t triggered by one thing-it’s triggered by dozens, and they vary wildly from person to person. Here are the six main categories of irritants that set off symptoms:- Environmental irritants: Tobacco smoke at just 0.05 mg/m³, perfume at 0.1 parts per million, paint fumes above 50 ppm of VOCs, and wildfire smoke (PM2.5 over 15 µg/m³) can all trigger a reaction. Even strong cleaning products or new carpet off-gassing can do it.
- Weather changes: A temperature drop of more than 5°C in an hour? That’s enough. Humidity shifts over 20%? Same thing. Barometric pressure drops of just 5 mmHg-like before a storm-can make your nose feel like it’s caving in.
- Food and drink: Spicy foods with capsaicin (think chili peppers) are a major trigger. Alcohol, even just one drink, can cause nasal stuffiness in many people. Cold drinks or hot soups can also provoke symptoms, especially in older adults. That’s called gustatory rhinitis.
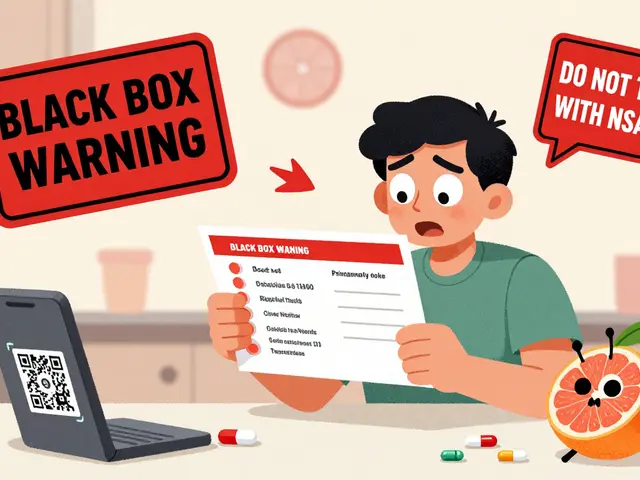
- Medications: High blood pressure drugs like ACE inhibitors (e.g., lisinopril) cause symptoms in 20% of users. Beta-blockers (like metoprolol) affect 15%. Even common NSAIDs like ibuprofen can trigger it in 10-15% of sensitive people. Hormone replacement therapy and birth control pills can also play a role.
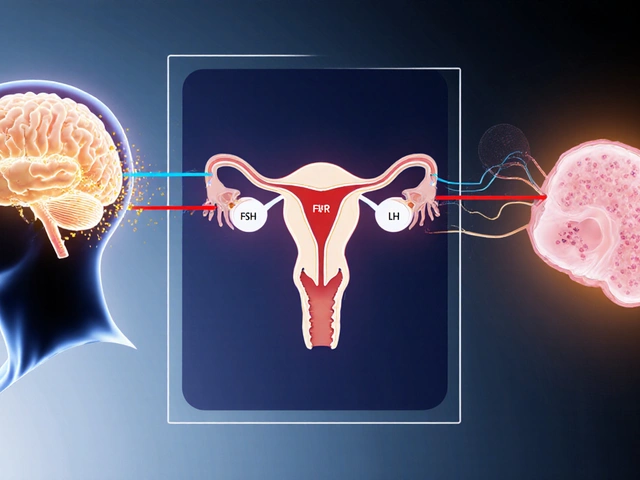
- Hormonal shifts: Pregnancy? Up to 30% of women develop rhinitis during the second trimester. Puberty and thyroid problems (especially hypothyroidism) can also cause nasal symptoms. These aren’t allergies-they’re hormonal changes messing with nasal blood flow.
- Workplace exposures: Flour dust (2 mg/m³), latex particles (over 2 µg/m³), chemical vapors, and even cleaning agents in hospitals or labs can trigger occupational rhinitis. Symptoms often worsen during the workweek and improve on weekends.
What’s wild is that these triggers don’t work the same for everyone. One person might react to cold air but not perfume. Another might be fine with smoke but break out in a runny nose every time they eat curry. That’s why tracking your own triggers is the first step to control.
How to Manage It: Real Strategies That Work
There’s no cure for nonallergic rhinitis, but you can take back control. Here’s what actually helps, based on clinical evidence-not guesswork.1. Avoid Your Triggers (It Sounds Simple, But It Works)
The most effective first step? Identify and reduce exposure. Use a symptom diary for 4-6 weeks. Write down:- Temperature and humidity (use a cheap indoor monitor)
- What you ate or drank
- Any new products you used (perfume, detergent, cleaning spray)
- Medications you took
- Whether you were outdoors or in a new building
After a month, patterns emerge. Maybe you notice symptoms spike every time you walk into your office. Or after drinking red wine. Or when the heater turns on. Once you know your triggers, you can make changes:
- Switch to fragrance-free laundry detergent and body wash
- Use a HEPA air purifier in your bedroom (they capture 99.97% of particles 0.3 microns and larger)
- Keep windows closed on windy days or when wildfire smoke is in the air
- Wear a mask when cleaning or gardening
- Avoid spicy foods if they trigger you
Studies show trigger avoidance alone can reduce symptoms by 25-40%.
2. Nasal Saline Irrigation
This is one of the most underused, yet highly effective tools. Rinsing your nose with saline (salt water) flushes out irritants, reduces inflammation, and improves mucus flow.Use either isotonic (0.9% salt) or hypertonic (3% salt) saline. Hypertonic works better for congestion. Do it twice a day-once in the morning and once before bed. Use a neti pot, squeeze bottle, or nasal spray. Make sure you use distilled, sterile, or boiled water. Tap water can carry dangerous microbes.
Research shows 60-70% of people get symptom relief. Twice-daily use is 45% more effective than once a day. Many users report improved sense of smell and less need for medication.
3. Intranasal Corticosteroids
If avoidance and saline aren’t enough, the next step is a nasal steroid spray. Fluticasone (Flonase), mometasone (Nasonex), or budesonide (Rhinocort) are first-line prescriptions.They reduce inflammation in the nasal lining. But here’s the catch: they don’t work right away. You need to use them daily for 2-4 weeks before seeing full results. Don’t give up after three days. They’re not decongestants-they’re anti-inflammatories.
Studies show they reduce symptoms by 50-60% in moderate to severe cases. Side effects? Minor nosebleeds in 15-20% of users. That’s usually from spraying too hard or too close to the septum. Aim the spray away from the center of your nose, toward your ear.
4. Ipratropium Bromide (Atrovent Nasal Spray)
This is the secret weapon for runny nose. If your main problem is dripping, not stuffiness, this is your go-to.Ipratropium is an anticholinergic. It blocks the nerve signals that make your nose leak. It starts working in 48 hours. By two weeks, it reduces rhinorrhea by 70-80%. It doesn’t help with congestion or sneezing-but if you’re constantly wiping your nose or soaking through tissues, it’s a game-changer.
It’s safe for long-term use. No addiction risk. No rebound congestion. Side effects? Dry nose or mild nosebleeds. A few people report a bitter taste, but that’s rare.
5. Antihistamine Nasal Sprays (Azelastine)
You’d think antihistamines wouldn’t work for nonallergic rhinitis. But azelastine (Astelin, Astepro) does help-just not as much as for allergies. It reduces overall symptoms by 30-40%. It starts working in 1-2 hours. The downside? It can cause a bitter taste in 30-40% of users. Some people also feel drowsy.It’s not a first-line treatment, but it’s useful if you’ve tried the others and still have some sneezing or itching.

What Doesn’t Work (And Why)
Many people waste time and money on things that don’t help. Here’s what to skip:- Oral antihistamines: Like loratadine or cetirizine. They’re useless for nonallergic rhinitis. No histamine is being released, so blocking it does nothing. Yet doctors still prescribe them by default.
- Decongestant nasal sprays (oxymetazoline, phenylephrine): These give quick relief-but only for 3-5 days. After that, you get rebound congestion (rhinitis medicamentosa). Your nose becomes dependent. Withdrawal can take 7-10 days and feels awful. Avoid these unless under medical supervision.
- Allergy shots: Immunotherapy won’t help because you’re not allergic. It’s a waste of time and money.
When to See a Specialist
Most people wait years to get a proper diagnosis. On Reddit’s r/allergies, 78% of nonallergic rhinitis patients reported a delay of over 3 years. 65% were misdiagnosed with allergies first.See an ENT or allergist if:
- Your symptoms last longer than 3 months
- Over-the-counter allergy meds don’t help
- You’re using decongestant sprays for more than 3 days at a time
- You have facial pain, nosebleeds, or loss of smell
They’ll do a nasal endoscopy and allergy testing. That’s how you get the right diagnosis. Once you know it’s nonallergic, you can stop chasing the wrong treatment.

What’s Coming Next
The future looks promising. Researchers are developing drugs that target TRPV1 receptors-the overactive sensors in your nose that react to heat, cold, and chemicals. A new TRPV1 blocker called BCT-100 showed 55% symptom reduction in phase 2 trials.There’s also early work on tiny nerve-stimulating devices that can calm the overactive signals in your nose. One pilot study at Johns Hopkins showed a 45% reduction in symptoms after just a few weeks of treatment.
And in March 2023, the FDA approved a new, lower-dose version of ipratropium (0.03%) that works just as well but causes fewer side effects.
Real People, Real Results
On Drugs.com, 62% of users who tried ipratropium said it gave them a "dramatic reduction" in runny nose within 24 hours. On Healthgrades, nasal saline irrigation got a 4.0/5 rating, with users saying it reduced their need for meds and brought back their sense of smell.But many still struggle. In a Facebook support group with 12,500 members, 68% said they’re frustrated by triggers they can’t control. 82% said doctors don’t understand their condition.
Successful management comes down to three things:
- Knowing your triggers
- Using saline and nasal steroids consistently
- Avoiding the trap of decongestant sprays
It’s not glamorous. But it works. And for the first time, you’re not chasing an allergy that doesn’t exist-you’re managing a real, treatable condition.
Is nonallergic rhinitis the same as allergies?
No. Allergies involve your immune system reacting to substances like pollen or pet dander, releasing histamine. Nonallergic rhinitis has no immune involvement. It’s caused by nerve sensitivity in the nose reacting to irritants like smoke, cold air, or perfumes. Allergy tests will come back negative.
Can I use antihistamines like Claritin for nonallergic rhinitis?
Oral antihistamines like Claritin or Zyrtec won’t help. Since there’s no histamine release in nonallergic rhinitis, blocking it does nothing. Nasal antihistamines like azelastine can help a little with sneezing and runny nose, but they’re not as effective as saline or ipratropium.
Why does my nose run when I eat spicy food?
That’s called gustatory rhinitis, a subtype of nonallergic rhinitis. Spicy foods contain capsaicin, which activates TRPV1 receptors in your nose. These receptors trigger nerve signals that cause your nasal glands to leak fluid. It’s not an allergy-it’s a reflex. It’s more common in older adults.
Is it safe to use nasal saline every day?
Yes. Daily nasal saline irrigation is not only safe-it’s recommended. Use distilled, sterile, or boiled water to avoid infection. Twice-daily use is more effective than once. Many users find it reduces their need for medications and improves breathing and smell over time.
Can pregnancy cause a runny nose?
Yes. Hormonal rhinitis affects 20-30% of pregnant women, especially in the second trimester. Rising estrogen levels cause nasal blood vessels to swell. Symptoms usually resolve within two weeks after delivery. It’s not an allergy and doesn’t harm the baby.
What’s the best way to avoid triggers in winter?
Use a humidifier to keep indoor humidity above 40%, wear a scarf over your nose when going outside, avoid sudden temperature changes, and skip strong scents like winter candles or fireplace smoke. Keep windows closed on windy days to keep cold, dry air out.
Do I need to stop my blood pressure medication if it causes rhinitis?
Don’t stop your medication without talking to your doctor. ACE inhibitors cause rhinitis in 20% of users, but they’re important for heart health. Ask your doctor about switching to a different class of blood pressure drug, like an ARB (e.g., losartan), which rarely causes this side effect.
How long does it take for nasal steroids to work?
Nasal steroids like Flonase take 2-4 weeks of daily use to reach full effect. Don’t stop after a few days. Use them consistently, even if you feel fine. They reduce inflammation over time, not instantly.
Next Steps
Start today. Buy a saline rinse kit and a simple indoor thermometer/hygrometer. Track your symptoms for two weeks. Identify your top three triggers. Talk to your doctor about ipratropium if you have a runny nose, or a nasal steroid if you’re congested. Skip the oral antihistamines and decongestant sprays.You don’t have to live with a constant runny nose. Nonallergic rhinitis is frustrating, but it’s manageable. And now, you know exactly how to take control.



Chris porto
December 18, 2025 AT 21:10Been dealing with this for years. Didn't even know it had a name until last month. My nose runs every time I walk into my office. Turned out to be the new carpet and the air purifier they installed. Switched to fragrance-free stuff and started saline rinses. Best decision ever.
Still can't eat curry without a full-on nasal flood though. Guess I'm just a spicy food casualty.
Frank Drewery
December 20, 2025 AT 17:29Saline rinses changed my life. I used to go through a box of tissues a day. Now I feel like I can actually breathe again. Takes a minute to get used to, but once you do, it's like your nose finally remembers how to be normal.
shivam seo
December 21, 2025 AT 18:38Wow. Another article telling people to rinse their nose with salt water. Groundbreaking. Meanwhile, the real issue is that our air is poisoned by corporate pollutants and government-approved chemicals. No one talks about that. You think your nose is sensitive? Try living in a country that lets Big Pharma sell you decongestants while ignoring the real toxins.
Andrew Kelly
December 22, 2025 AT 09:50Let me guess - you’re all for saline rinses and nasal sprays, but what about the truth? The FDA approved ipratropium in 2023 because they’re hiding something. There’s a reason they pushed this as a ‘nonallergic’ condition. It’s not about irritants. It’s about the vaccines. The neurological side effects are being buried under buzzwords like ‘vasomotor rhinitis.’
Ask yourself: why did this spike right after 2020? Why do all the ‘experts’ avoid the elephant in the room? I’ve seen the data. It’s not coincidence.
Ashley Bliss
December 22, 2025 AT 12:39I used to think I was just dramatic. Like my nose was a broken faucet and I was the sad person who couldn’t fix it. Then I found out it wasn’t me - it was the world. The perfume, the cold air, the wine I loved… all of it was attacking me. And no one believed me.
Now I cry when I use my neti pot. Not because it hurts. Because for the first time, I’m not broken. I’m just… sensitive. And that’s okay.
Dev Sawner
December 23, 2025 AT 15:22It is imperative to underscore that the management of nonallergic rhinitis must adhere strictly to evidence-based protocols. The utilization of hypertonic saline irrigation at a concentration of 3% sodium chloride, administered bid, demonstrates statistically significant reduction in mucosal edema (p < 0.01). Furthermore, the off-label use of intranasal corticosteroids is not only clinically validated but also cost-effective when compared to prolonged oral antihistamine regimens, which are physiologically inert in this context.
It is regrettable that laypersons continue to propagate misinformation regarding the efficacy of immunotherapy in non-IgE-mediated conditions. Such misconceptions perpetuate diagnostic delays and increase healthcare burden.
Mahammad Muradov
December 24, 2025 AT 17:48Most people don’t realize that gustatory rhinitis is a direct result of TRPV1 receptor overexpression. Capsaicin activates these receptors, which are densely concentrated in the nasal mucosa. This is not a ‘reflex’ - it’s neurogenic inflammation. The same mechanism applies to cold air and perfumes. The body isn’t allergic - it’s hyperinnervated.
And yes, ACE inhibitors cause this because they increase bradykinin. That’s why ARBs don’t. Simple pharmacology. Stop blaming everything on the environment. Your medication is the trigger.
Takeysha Turnquest
December 25, 2025 AT 21:12I didn’t know I was crying every time I ate soup until I started tracking it. Turns out I was. Every. Single. Day. And no one ever said it was okay to be this broken. Now I rinse. I avoid. I breathe. And for the first time in years, I feel like I’m not just surviving - I’m living.
Thank you for writing this. I needed to hear it.