Not all diabetes pills are created equal
When you’re first diagnosed with type 2 diabetes, your doctor might hand you a prescription for metformin and say, "Take this twice a day." But what if that pill gives you stomach cramps so bad you stop taking it? Or what if another drug helps your blood sugar but makes you gain weight or causes frequent infections? The truth is, choosing diabetes medications isn’t just about lowering A1C-it’s about matching the drug to your body, your life, and your tolerance for side effects.
Metformin: The starter pill with a rough start
Metformin is still the most prescribed first-line treatment for type 2 diabetes, used by over 42% of new patients. Why? It’s cheap, doesn’t cause weight gain, and rarely leads to low blood sugar. But here’s the catch: nearly 30% of people get stomach issues-diarrhea, nausea, bloating-right after starting it. That’s not just uncomfortable; it’s why so many quit.
The fix? Start low. Take 500 mg once a day with your evening meal. Wait a week, then bump it to 500 mg twice a day. Most people can work up to 2,000 mg daily without major problems if they go slow. Switching to the extended-release version cuts GI side effects in half. One study showed 82% of users who switched from regular metformin to extended-release said they could finally stick with it.
Metformin is safe for most people, but if your kidney function drops below an eGFR of 30, you need to stop. It’s rare, but lactic acidosis can happen in people with severe kidney disease or those who drink heavily. For most, though, it’s the safest bet to begin with.
Sulfonylureas: Effective-but risky
Drugs like glimepiride and glibenclamide have been around for decades. They work well to lower blood sugar, but they’re like a blunt tool: they force your pancreas to pump out insulin no matter what. That’s why hypoglycemia is so common.
Here’s the scary part: glibenclamide causes low blood sugar in 77% of users. Glimepiride? Still high at 44%. That’s more than double the risk compared to newer drugs. Older adults, people with irregular meals, or those who drive for a living are at serious risk. One study found 72% of people who quit sulfonylureas did so because of low blood sugar episodes-some so bad they ended up in the ER.
Weight gain is another issue. Glimepiride causes about 26% of users to gain weight. Glibenclamide? Less weight gain, but more hypoglycemia. If you’re trying to lose weight or already have heart issues, these aren’t ideal. Most experts now reserve them for people who can’t afford newer meds or have no other options.
SGLT-2 inhibitors: The heart and kidney protectors
Drugs like empagliflozin and dapagliflozin work by making your kidneys dump sugar out in your urine. Sounds weird, right? But the side effects are manageable-and the benefits are huge.
They lower your risk of heart failure hospitalizations by up to 30%. They slow kidney disease progression. And they help you lose weight-on average, 5-8 pounds over six months. But here’s the trade-off: genital yeast infections. About 8-11% of women and 1-4% of men get them. It’s not dangerous, but it’s annoying. The fix? Good hygiene. Wipe front to back, wear cotton underwear, and don’t sit in wet swimsuits. Most cases clear up with over-the-counter antifungal cream.
Some people feel lightheaded when they start, especially if they’re on diuretics or have low blood pressure. That’s because these drugs pull fluid out of your body. Drink more water. Don’t skip meals. If you feel dizzy, talk to your doctor about adjusting other meds.
There’s also a rare but serious risk: Fournier’s gangrene, a life-threatening genital infection. It’s happened in about 0.002% of users. The FDA now requires warning labels, but the actual risk is extremely low. For people with heart or kidney disease, the benefits far outweigh this tiny risk.
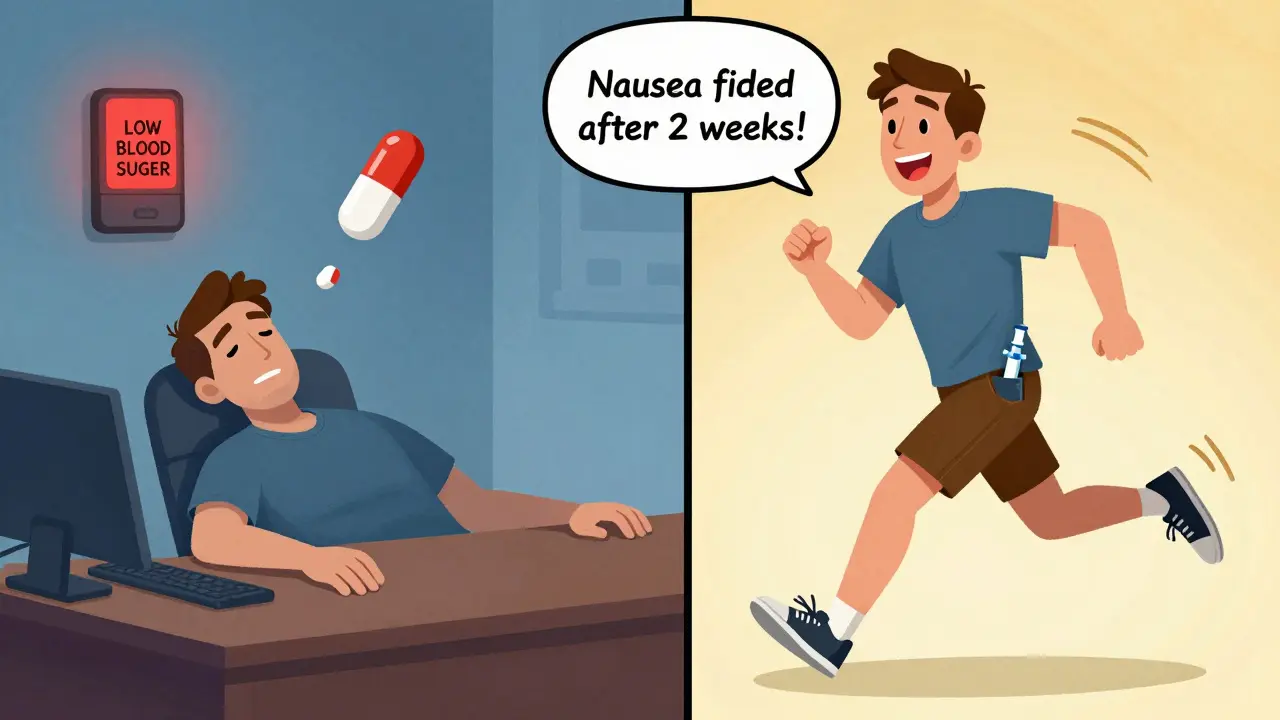
GLP-1 receptor agonists: Weight loss with a side of nausea
Liraglutide, semaglutide, and tirzepatide are injectables that mimic a gut hormone. They slow digestion, reduce appetite, and help your pancreas release insulin only when needed. That means less hypoglycemia and major weight loss-up to 15 pounds or more in six months.
The downside? Nausea. Up to 45% of people feel sick when they start. Vomiting and diarrhea are common too. But here’s the good news: 74% of people who stuck with it past eight weeks said the nausea faded. The trick? Start with the lowest dose. Wait four weeks before increasing. Most people adjust without quitting.
These drugs are now recommended as first-line for people with obesity (BMI ≥30) or heart disease. In fact, prescriptions for GLP-1 agonists jumped from 9% of new diabetes prescriptions in 2018 to 24% in 2022. Why? Because they don’t just treat diabetes-they improve your overall health.
Tirzepatide (Mounjaro), the newest, combines GLP-1 with GIP. In trials, it caused 15.7% weight loss at the highest dose-with nausea rates lower than semaglutide. It’s not cheap, but for many, the results are life-changing.
DPP-4 inhibitors: The quiet option
Sitagliptin, linagliptin, saxagliptin-these are oral pills that boost your body’s own GLP-1. They’re mild. They don’t cause weight gain. Hypoglycemia risk is low unless you’re taking them with sulfonylureas.
The side effects? Mostly mild: stuffy nose, headache, sore throat. About 12% of users report nasopharyngitis. A small number (8.4%) say they get joint pain. That’s why some stop.
What makes them stand out? Kidney safety. Linagliptin doesn’t need dose adjustments even if your kidneys are weak. Saxagliptin does-cut the dose in half if your eGFR is below 50. If you have kidney disease and can’t take metformin, DPP-4 inhibitors are one of the safest oral options left.
Thiazolidinediones: The forgotten class
Pioglitazone and rosiglitazone improve insulin sensitivity. But they’re rarely used now-and for good reason.
Rosiglitazone was pulled from the European market in 2010 after studies linked it to a 30-40% higher risk of heart attacks. Pioglitazone is still available, but it carries a 27% higher risk of bladder cancer after two years of use at high doses (over 80 mg/day). If you’ve had bladder cancer, or have blood in your urine, or are a smoker, avoid it.
It also causes fluid retention, which can worsen heart failure. And it increases bone fracture risk by 50% compared to metformin-especially in older women.
These are not first-line. They’re only considered in rare cases where other drugs failed, and the patient has no history of cancer, heart failure, or osteoporosis.
How to choose: Your side effect checklist
Here’s a simple way to think about it:
- Want to lose weight? GLP-1 agonists or SGLT-2 inhibitors.
- Have heart or kidney disease? SGLT-2 inhibitors or GLP-1 agonists.
- Worried about low blood sugar? Avoid sulfonylureas. Choose metformin, DPP-4 inhibitors, or GLP-1 agonists.
- Have stomach issues? Start with extended-release metformin. Avoid GLP-1s until you’re ready for nausea.
- Have kidney problems? Avoid metformin if eGFR <30. Use linagliptin or SGLT-2 inhibitors (check dosage).
- On a tight budget? Metformin and sulfonylureas are cheapest-but weigh the long-term risks.
There’s no one-size-fits-all. What works for your neighbor might make you sick. Your doctor should ask: "What are you most afraid of?" Is it fainting from low blood sugar? Gaining weight? Getting infections? That’s your starting point.
Real people, real choices
On Reddit, one user wrote: "I stopped metformin because I couldn’t leave the house. Switched to semaglutide-nausea for two weeks, then it vanished. Lost 22 pounds. My A1C dropped from 8.9 to 5.7. Best decision I ever made."
Another said: "I was on empagliflozin. Got yeast infections every month. I started wearing cotton underwear and changed out of wet clothes right after swimming. No more infections. My heart feels better. I keep taking it."
And one who quit sulfonylureas: "I passed out at work three times in six months. My boss thought I was drunk. I was just low. Switched to metformin and GLP-1. Never had another episode."
These aren’t outliers. They’re the norm.
What’s next? Better drugs are coming
Researchers are working on "smart insulins" that only activate when blood sugar is high-no more low blood sugar. There are also microbiome-targeted pills designed to reduce metformin’s stomach upset. One pilot study showed a probiotic supplement cut diarrhea by 40%.
By 2028, over half of all diabetes meds will be chosen because they help you lose weight or protect your heart-not just because they lower sugar. That’s the future: treatment that fits your life, not the other way around.
Which diabetes medication has the least side effects?
Metformin (extended-release) and DPP-4 inhibitors like linagliptin have the mildest side effect profiles overall. Metformin causes stomach issues in about 30% of users, but that drops to under 10% with the extended-release version. DPP-4 inhibitors rarely cause low blood sugar or weight gain, and most side effects are mild-like a stuffy nose or headache. They’re often the best choice for people who want to avoid major side effects.
Can I switch diabetes meds if the side effects are too bad?
Yes, absolutely. Many people stop their first diabetes medication because of side effects-and that’s normal. Don’t suffer in silence. Talk to your doctor. There are at least five other classes of drugs to try. For example, if metformin gives you diarrhea, switch to extended-release. If you’re getting yeast infections from an SGLT-2 inhibitor, try a GLP-1 agonist instead. Treatment is personalized. You’re not stuck with the first pill you’re given.
Do all diabetes drugs cause weight gain?
No. Sulfonylureas and thiazolidinediones (like pioglitazone) often cause weight gain-up to 10 pounds or more. But metformin, DPP-4 inhibitors, SGLT-2 inhibitors, and GLP-1 agonists either cause no weight gain or help you lose weight. GLP-1 agonists like semaglutide and tirzepatide can lead to 10-20 pounds of weight loss over six months. If weight is a concern, avoid sulfonylureas and choose drugs that support weight loss.
Why do some people get yeast infections on SGLT-2 inhibitors?
SGLT-2 inhibitors make your kidneys remove sugar through urine. That sugar ends up in your genital area, creating a perfect environment for yeast to grow. Women are more likely to get infections than men. The good news? These are treatable with over-the-counter antifungal creams or suppositories. Keeping the area clean and dry, wearing cotton underwear, and changing out of wet clothes quickly can reduce the risk by up to 35%.
Is it safe to take metformin if I have kidney problems?
Metformin is not safe if your kidney function is severely reduced (eGFR below 30 mL/min). At that level, your body can’t clear the drug properly, which increases the risk of lactic acidosis. If your eGFR is between 30 and 45, your doctor may lower your dose. If it’s above 45, metformin is usually fine. Always get your kidney function checked before starting or continuing metformin. If your kidneys are weak, DPP-4 inhibitors like linagliptin or SGLT-2 inhibitors are safer alternatives.
What’s the best diabetes medication for older adults?
For older adults, the goal is to avoid low blood sugar and keep things simple. Metformin (if kidneys are okay) or DPP-4 inhibitors like linagliptin are preferred. Avoid sulfonylureas like glimepiride or glibenclamide-they cause too many dangerous low blood sugar episodes in older people. GLP-1 agonists can be used too, but nausea might be harder to tolerate. The key is choosing a drug that doesn’t require frequent meals or complex dosing, and doesn’t put you at risk of fainting or falls.






Heather McCubbin
January 22, 2026 AT 13:38Stop being dramatic. Start slow. It works.
Dolores Rider
January 24, 2026 AT 00:50venkatesh karumanchi
January 24, 2026 AT 21:25John McGuirk
January 25, 2026 AT 21:07Michael Camilleri
January 26, 2026 AT 06:49Also stop blaming the drug. Blame your impatience.
lorraine england
January 27, 2026 AT 14:50Darren Links
January 28, 2026 AT 10:09Kat Peterson
January 29, 2026 AT 14:31Izzy Hadala
January 29, 2026 AT 23:57Elizabeth Cannon
January 30, 2026 AT 11:37Marlon Mentolaroc
January 30, 2026 AT 18:02Phil Maxwell
January 31, 2026 AT 22:35Karen Conlin
February 2, 2026 AT 08:30asa MNG
February 3, 2026 AT 04:32Sushrita Chakraborty
February 5, 2026 AT 00:11