Every year, millions of older adults take over-the-counter allergy or sleep meds like Benadryl without realizing they’re stacking up a hidden danger. It’s not just one pill. It’s the antihistamines they take for allergies, plus the sleep aid, the bladder pill, the antidepressant, and maybe even the motion sickness tablet-all adding up to something called cumulative anticholinergic burden. And for people over 65, this buildup isn’t just a side effect. It’s a silent threat to memory, balance, and independence.
What Is Cumulative Anticholinergic Burden?
Anticholinergic drugs block acetylcholine, a brain chemical that helps with memory, muscle control, and organ function. When you take one medication with this effect, your body can handle it. But when you take several-especially over months or years-the effects pile up. This is the cumulative anticholinergic burden. It’s not about how strong each drug is alone. It’s about how they work together.
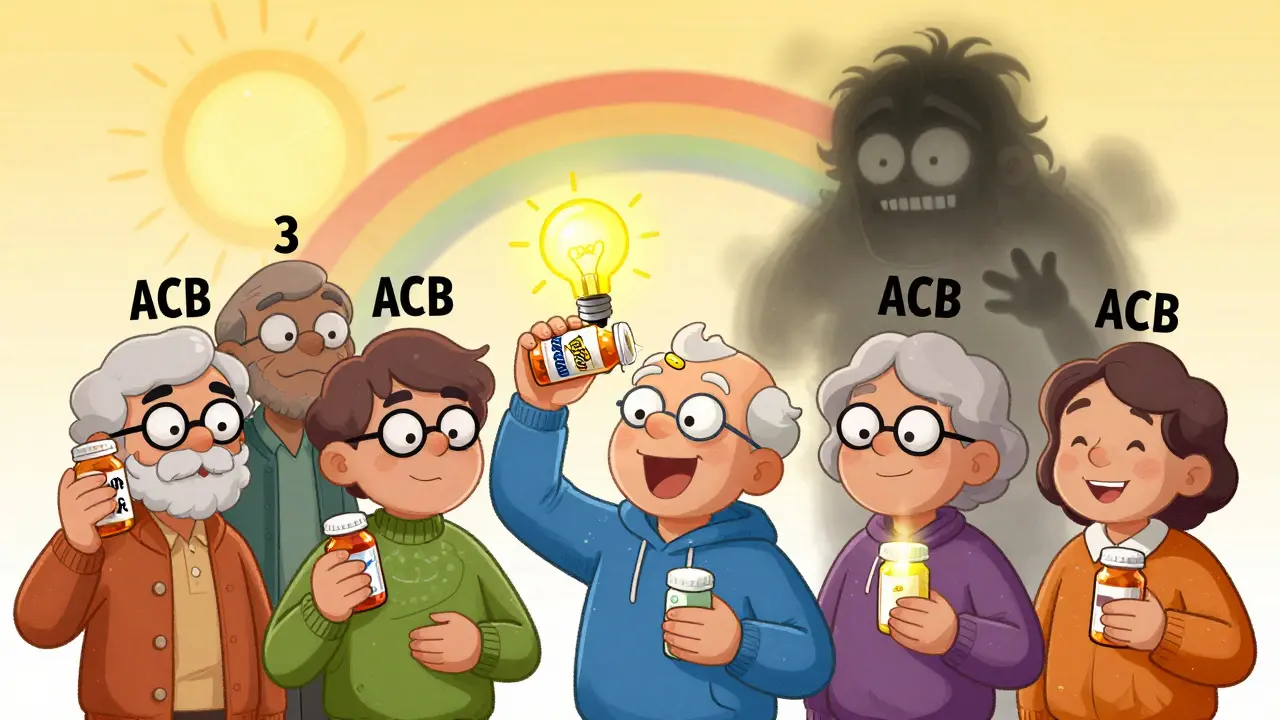
The most widely used tool to measure this is the Anticholinergic Burden (ACB) Scale. Developed in 2008, it scores medications from 0 to 3:
- Score 0: No anticholinergic effect
- Score 1: Mild effect (like some diuretics or second-gen antihistamines)
- Score 2-3: Strong effect (like diphenhydramine, amitriptyline, or oxybutynin)
If your total ACB score hits 3 or higher, your risk of cognitive decline, falls, urinary retention, and even dementia jumps significantly. A 2015 study in JAMA Internal Medicine followed over 3,400 people for seven years and found those taking strong anticholinergics for more than three years had a 54% higher risk of dementia.
Why Antihistamines Are a Major Player
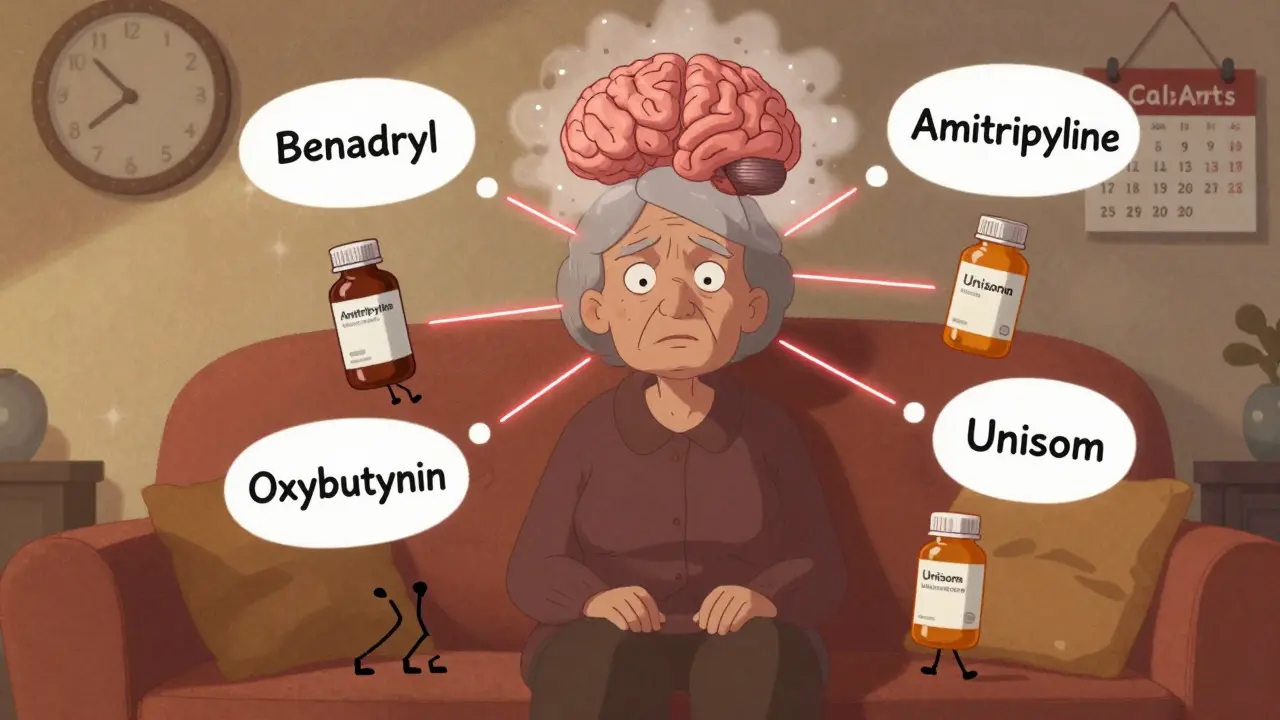
Not all antihistamines are the same. First-generation ones-like diphenhydramine (Benadryl), chlorpheniramine (Chlor-Trimeton), and doxylamine (Unisom)-are strong anticholinergics. They cross the blood-brain barrier and directly interfere with memory circuits. These are the ones sold in sleep aids and allergy pills. Many people use them nightly for years without knowing the long-term cost.
Second-generation antihistamines-like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra)-have almost no anticholinergic effect. They’re designed to stay out of the brain. So if you’re taking Benadryl every night for sleep, switching to Claritin for allergies and melatonin for sleep could cut your ACB score in half.
Here’s the scary part: 40% of the total anticholinergic burden in older adults comes from medications people don’t even think of as anticholinergic. That includes bladder medications, antidepressants, Parkinson’s drugs, and yes-over-the-counter antihistamines. A 2021 study from NPS MedicineWise found that just one other anticholinergic drug added to a daily antihistamine often pushes the total ACB score over 3.

Common Medications That Add Up
Let’s look at real examples of how these drugs combine. A typical older adult might be taking:
- Diphenhydramine (Benadryl) 25 mg nightly for sleep → ACB score 3
- Amitriptyline 25 mg for nerve pain → ACB score 3
- Oxybutynin 5 mg for overactive bladder → ACB score 3
Add those up: 3 + 3 + 3 = 9. That’s not just risky. That’s dangerous.
Even if someone isn’t on three strong drugs, combinations like this are common:
- Diphenhydramine + amitriptyline → ACB 6
- Chlorpheniramine + oxybutynin → ACB 6
- Doxylamine + benztropine (Parkinson’s drug) → ACB 5
And here’s what makes it worse: most people don’t realize their OTC meds count. A 2022 survey on AgingCare.com found that 7 out of 10 caregivers said their doctor never warned them that allergy pills could affect memory. Yet, these are the exact pills that contribute the most to the burden.
Who’s Most at Risk?
Older adults are the most vulnerable-not because they’re frail, but because their bodies process drugs differently. Kidney and liver function decline with age. The brain becomes more sensitive to acetylcholine disruption. And most take five or more medications daily. According to the American Geriatrics Society’s 2020 Beers Criteria, 20-50% of older adults are exposed to at least one anticholinergic drug.
Women over 65 are especially at risk because they’re more likely to be prescribed bladder medications and antidepressants. People with Parkinson’s, chronic allergies, or insomnia are often on multiple anticholinergics without realizing the connection.
And the effects aren’t subtle. Symptoms include:
- Confusion or memory lapses mistaken for dementia
- Frequent falls or unsteadiness
- Blurred vision
- Constipation or urinary retention
- Dry mouth and drowsiness
One Reddit user shared that their 78-year-old mother was diagnosed with early dementia-until they stopped her nightly Benadryl and amitriptyline. Within six weeks, her memory improved. Her ACB score dropped from 4 to 1.
How to Reduce the Burden
You don’t have to stop all medications. You just need to know what’s contributing and swap out the high-risk ones.
Here’s a practical 4-step plan:
- Review every medication-prescription and OTC. Write down everything you take, even herbal supplements.
- Check the ACB score for each. You can find free lists online from the IU Center for Aging Research or NPS MedicineWise.
- Swap strong anticholinergics for safer alternatives:
- Replace diphenhydramine (Benadryl) with melatonin or cognitive behavioral therapy for sleep.
- Replace chlorpheniramine with loratadine or cetirizine for allergies.
- Replace oxybutynin with mirabegron (a non-anticholinergic bladder drug).
- Replace amitriptyline with SSRIs like sertraline for depression or nerve pain.
And here’s the good news: studies show that when people make these switches, their cognitive function improves. A case study in NPS MedicineWise’s 2021 report showed a 72-year-old patient with an ACB score of 5 regained balance, reduced falls by 75%, and improved mental clarity after six months of deprescribing.
Many primary care clinics now use automated alerts in electronic health records. If your ACB score hits 3, the system flags it. But if your doctor doesn’t ask about OTC meds, you need to speak up.
What You Can Do Today
Don’t wait for a crisis. Take action now:
- Ask your pharmacist: “Which of my medications have anticholinergic effects?”
- Bring your pill bottle list to your next appointment. Don’t rely on memory.
- Ask: “Can this be replaced with a non-anticholinergic option?”
- Stop using OTC sleep aids with diphenhydramine or doxylamine. Try melatonin, sleep hygiene, or a sleep specialist instead.
The FDA added warnings to first-generation antihistamine labels in 2017. The European Medicines Agency followed in 2019. And in 2023, the American Geriatrics Society updated its guidelines to say: “Chronic use of first-generation antihistamines should be avoided in older adults due to strong evidence of cognitive impairment even at low doses.”
This isn’t about fear. It’s about awareness. You don’t need to stop all meds. You just need to know which ones are quietly hurting you-and replace them with safer choices.
Can antihistamines really cause dementia?
Yes, long-term use of strong anticholinergic antihistamines like diphenhydramine has been linked to a 54% higher risk of dementia in people over 65 who use them for more than three years, according to a landmark 2015 JAMA study. This doesn’t mean every person who takes Benadryl will get dementia-but the risk increases significantly with cumulative exposure. The effect is dose- and time-dependent. Stopping these drugs can reverse some cognitive decline.
Are all allergy pills the same?
No. First-generation antihistamines like Benadryl, Chlor-Trimeton, and Unisom have strong anticholinergic effects (ACB score 2-3). Second-generation ones like Claritin, Zyrtec, and Allegra have minimal to no effect (ACB score 0-1). If you take allergy meds daily, switch to a second-generation option. They’re just as effective for allergies and don’t fog your brain.
I take Benadryl to help me sleep. What should I use instead?
Melatonin (1-3 mg) taken 30-60 minutes before bed is a safer, non-anticholinergic option. Cognitive behavioral therapy for insomnia (CBT-I) is even more effective long-term. If you need something stronger, talk to your doctor about non-sedating sleep aids. Never combine antihistamines with other sedatives like alcohol or benzodiazepines-that’s a dangerous mix.
How do I know if my meds are adding up?
Use the ACB Scale. List every medication you take daily, including OTCs. Check each one’s score online (search “ACB Scale list 2026”). Add them up. If the total is 3 or more, talk to your doctor about deprescribing. Even if you feel fine, the damage may already be happening silently.
Is this only a problem for older adults?
The highest risk is in people over 65 because their bodies process drugs slower and their brains are more sensitive. But younger people with chronic conditions (like Parkinson’s or severe allergies) who take multiple anticholinergics long-term can also be at risk. It’s not age alone-it’s cumulative exposure. The longer you take them, the higher the risk.




Sarah Barrett
February 15, 2026 AT 00:09It’s staggering how many of us are walking around with brain fog and never connect it to that nightly Benadryl or that ‘harmless’ bladder pill. I’ve seen it in my mother-in-law-suddenly forgetful, clumsy, irritable-and no one thought to look at her medication list. The ACB scale is a revelation. It’s not magic, it’s math. And math doesn’t lie. Swapping out diphenhydramine for melatonin didn’t just improve her sleep-it restored her laughter. That’s not a side effect. That’s a life reclaimed.
Josiah Demara
February 16, 2026 AT 12:15Let’s be brutally honest: this isn’t a medical issue-it’s a societal failure. People treat OTC meds like candy. They don’t read labels, they don’t ask questions, and they certainly don’t care about pharmacokinetics. A 54% increased dementia risk? That’s not a whisper-it’s a siren. And yet, pharmacies still stock Benadryl next to gum and candy bars. The FDA warning? Too little, too late. The real tragedy? It’s entirely preventable. If you’re over 65 and still using diphenhydramine as a sleep aid, you’re not just risking your brain-you’re insulting your own intelligence.
Kaye Alcaraz
February 18, 2026 AT 09:57Knowledge is power, and this post is a gift. Thank you for laying out the science with such clarity. I’ve shared this with my entire book club-women over 65, all on multiple meds. We’re scheduling a pharmacist consult next week. One woman switched from oxybutynin to mirabegron and hasn’t had a fall in three months. Small changes. Huge impact. Let’s stop seeing this as a ‘senior problem’ and start seeing it as a ‘human health opportunity.’
Charlotte Dacre
February 20, 2026 AT 03:20Oh, so now we’re blaming Benadryl for dementia? How convenient. Next you’ll tell me that breathing air causes Alzheimer’s. People have been taking this stuff for decades. If your grandma’s memory faded after 20 years of nighttime NyQuil, maybe she was just aging. Or maybe-just maybe-your obsession with ‘ACB scores’ is just another way to sell supplements.
Chiruvella Pardha Krishna
February 20, 2026 AT 12:18In the grand tapestry of human existence, the accumulation of chemical burdens is but a reflection of our disconnection from natural rhythms. The body, like a river, was never meant to be dammed by synthetic molecules. To reduce anticholinergic burden is not merely to swap pills-it is to reawaken the ancient wisdom of stillness, of silence, of surrender to the body’s own intelligence. The pill is a symptom. The cure lies in the silence between breaths.
Virginia Kimball
February 22, 2026 AT 11:48I switched from Benadryl to melatonin last year and honestly? My brain feels lighter. Like someone turned off a fog machine inside my skull. I didn’t even know I was so foggy until it was gone. And yes, I still take my blood pressure med and my nerve pain pill-but now I check every single one on the ACB list. It’s like cleaning out a closet you didn’t know was full of dust. Simple. Free. Life-changing.
Kapil Verma
February 22, 2026 AT 16:50This is what happens when you let Western medicine become a religion. In India, we’ve used natural remedies for centuries-turmeric, ashwagandha, neem. No one here takes diphenhydramine for sleep. We sleep because we’re tired, not because we’ve been conditioned to swallow chemicals. This whole ACB nonsense? It’s Big Pharma’s way of making you dependent. Your body doesn’t need your pills-it needs your discipline. Stop relying on pills. Start relying on yourself.
Michael Page
February 24, 2026 AT 08:27The data is clear. The mechanisms are understood. The interventions are simple. Yet, the system does nothing. Why? Because profit > prevention. The real tragedy isn’t the dementia-it’s that we’ve normalized this slow erosion of cognition as ‘just part of getting old.’ We’ve stopped asking ‘why?’ and started accepting ‘because that’s how it is.’
Betty Kirby
February 24, 2026 AT 14:18Let’s not sugarcoat this. If you’re taking three or more anticholinergics and you’re over 65, you’re playing Russian roulette with your mind. And if you’re still using Benadryl as a sleep aid? You’re not just at risk-you’re already on the path. I’ve seen too many patients go from ‘a little forgetful’ to ‘doesn’t recognize her own daughter’ because no one bothered to ask about OTC meds. It’s not paranoia. It’s pattern recognition. And the pattern is lethal.
Erica Banatao Darilag
February 25, 2026 AT 17:09i just read this and i think its so important. my dad took benadryl for years and he started forgetting my name. we stopped it and he got better. i didnt know it was the medicine. i thought he was just getting old. thank you for writing this. i printed it out and gave it to my aunt. she was on 4 of these. now she’s switching. i hope more people see this.
Esha Pathak
February 26, 2026 AT 09:13Life is a balance, isn’t it? We take pills to sleep, to calm nerves, to empty bladders… but we forget the soul has its own rhythm. The brain is not a machine to be tuned with chemicals-it’s a garden. And when we flood it with anticholinergics, we choke the roots. The solution? Not just substitution, but surrender. To silence. To stillness. To the quiet wisdom of letting go. The pill is a bandage. The healing? It begins when we stop listening to the noise.