For decades, pharmacists were seen as the people who handed out pills - counted tablets, checked labels, and gave out cups of water. But that’s not the whole story anymore. Across the U.S., pharmacists are now legally allowed to do far more than just fill prescriptions. They can switch medications, start treatments, order tests, and even prescribe certain drugs - all without waiting for a doctor’s signature. This shift isn’t just a nice perk. It’s a response to real problems: too few doctors in rural towns, long waits for basic care, and patients skipping meds because they can’t afford a clinic visit. The question isn’t whether pharmacists should have more power. It’s what they can do, where, and how - and why it matters to you.
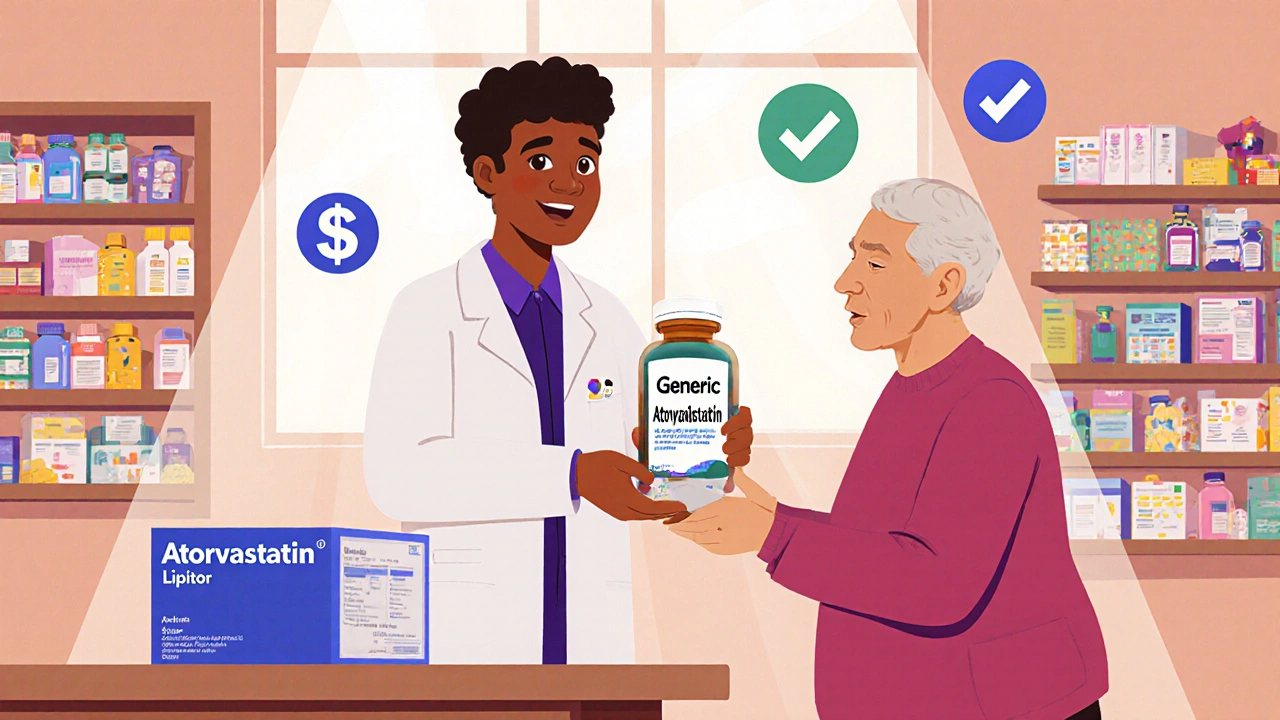
Generic Substitution: The Baseline Everyone Has
Every state lets pharmacists swap a brand-name drug for a cheaper generic version - as long as the doctor didn’t write "dispensed as written" on the prescription. This isn’t new. It’s been standard since the 1980s. But it’s still the most common form of substitution. The FDA requires generics to be chemically identical to the brand-name drug, with the same active ingredient, strength, and dosage form. That means if you’re on Lipitor and your pharmacist hands you atorvastatin, you’re getting the same medicine - just at a fraction of the cost. No permission needed. No paperwork. Just savings.
But here’s the catch: not all generics are created equal in patients’ eyes. Some people feel better on the brand. Others worry about side effects. That’s why pharmacists are required to tell you if a switch is happening. If you say no, they have to honor it. It’s your right.
Therapeutic Interchange: When Pharmacists Can Swap Different Drugs
Now things get more complex. Therapeutic interchange means a pharmacist can switch you to a different drug in the same class - not just a generic version. For example, if your doctor prescribes simvastatin for cholesterol, but your pharmacy’s formulary prefers pravastatin because it’s cheaper and has fewer side effects in older patients, the pharmacist can make the swap - if the law allows it.
As of 2025, only three states - Arkansas, Idaho, and Kentucky - have full therapeutic interchange laws. But they come with strict rules. In Kentucky, the doctor must write "formulary compliance approval" on the prescription. In Arkansas and Idaho, the prescriber must check a box saying "therapeutic substitution allowed." If they don’t, the pharmacist can’t change a thing. And even if they do, the pharmacist must call the doctor to let them know what was switched. In Idaho, they also have to sit down with you, explain the difference, and get your verbal consent. You can say no. And they have to document it all.
This isn’t about cutting corners. It’s about smart clinical judgment. A pharmacist might know that a different statin won’t interact with your other meds, or that a newer blood pressure pill has fewer dizziness side effects. They’re trained to spot those details.
Prescription Adaptation: Fixing a Prescription Without Calling the Doctor
Imagine you’re in a small town in New Mexico. Your doctor is 90 miles away. Your blood pressure meds were prescribed three months ago, but your last check-up showed your numbers are still high. You need a higher dose - but you can’t afford to take a day off work and drive that far.
In states that allow prescription adaptation, your pharmacist can adjust your dose - up or down - based on your latest lab results or blood pressure readings. They don’t need to call the doctor. They don’t need a new script. They just follow a pre-approved protocol set by the state board of pharmacy. This is common in rural states like New Mexico, Colorado, and Alaska. It’s not prescribing from scratch. It’s fine-tuning an existing plan.
The rules vary. Some states let pharmacists adjust diabetes meds. Others allow changes to thyroid or blood thinners. But there are limits. You can’t get antibiotics this way. You can’t get opioids. And you must have a recent medical history on file. The goal isn’t to replace your doctor. It’s to keep you on track when you can’t get to them.

Collaborative Practice Agreements: Pharmacists as Part of the Team
Every state allows Collaborative Practice Agreements (CPAs). These are formal, written contracts between a pharmacist and one or more doctors. They spell out exactly what the pharmacist can do - like starting a new medication, adjusting doses, ordering lab tests, or managing chronic conditions like asthma or diabetes.
CPAs aren’t new, but they’re growing fast. In 2025, 44 states introduced bills to expand them. In Minnesota, pharmacists can now manage anticoagulation therapy for patients on warfarin - adjusting doses based on INR results. In California, they can initiate flu shots and diabetes screenings under CPA protocols. In Washington, they can even prescribe nicotine patches and stop-smoking meds without a doctor’s direct involvement.
The key is structure. A CPA must define: who can be treated, what drugs can be used, what tests are allowed, when to refer to a doctor, and how to document everything in the electronic health record. It’s not a free-for-all. It’s a team approach - with pharmacists as full partners.
Independent Prescribing: The New Frontier
The most advanced states are moving toward independent prescribing - where pharmacists can start and stop medications without any doctor’s input, as long as they follow statewide protocols.
California lets pharmacists "furnish" emergency contraception, naloxone (for opioid overdoses), and birth control pills to adults without a prescription. Maryland lets pharmacists prescribe birth control to anyone over 18. Maine lets them prescribe nicotine replacement therapy. New Mexico and Colorado have statewide protocols that let pharmacists prescribe for conditions like strep throat, urinary tract infections, and allergic rhinitis - all without a doctor’s signature.
These aren’t random. They’re targeted. They’re for conditions that are common, well-understood, and low-risk. No one is handing out antibiotics for pneumonia or insulin for type 1 diabetes. But for a UTI? A pharmacist can test your urine, confirm the infection, and give you a 7-day course of antibiotics - all in 20 minutes. No appointment. No wait.
Why This Matters: Access, Equity, and Cost
There are 60 million Americans living in areas with too few doctors. Many of them are in rural towns, inner cities, or places with high poverty. In these areas, pharmacies are often the only health access point. If you can’t get to a clinic, you don’t get care. And if you don’t get care, your condition gets worse - and more expensive to treat.
Pharmacists are already there. They’re open evenings and weekends. They don’t require appointments. And they’re trained to catch drug interactions, spot overuse, and simplify regimens. When they’re allowed to act, they prevent hospitalizations. A 2023 study in the Journal of the American Pharmacists Association found that pharmacist-led anticoagulation management reduced emergency visits by 37% in rural communities.
It’s also about equity. Low-income patients are more likely to skip meds because of cost. Pharmacists can swap to cheaper alternatives, help apply for patient assistance programs, or even give out free samples. They’re the last line of defense against treatment abandonment.
The Pushback: Doctors, Corporations, and Reimbursement
Not everyone agrees. The American Medical Association still argues that pharmacists don’t have the same training as physicians. They worry about fragmentation of care - that patients might see a pharmacist for one issue and a doctor for another, and no one has the full picture.
There’s also corporate influence. Big pharmacy chains like CVS and Walgreens have spent millions lobbying for expanded authority. Critics say they’re pushing for more power to drive profits - not patient care. But the data doesn’t support that fear. Studies show pharmacist-led care improves outcomes regardless of who owns the store.
The real barrier? Money. Insurance companies don’t always pay pharmacists for these services. Even in states where pharmacists can prescribe, Medicaid and Medicare often don’t reimburse them. That’s why the federal ECAPS Act is so important. If passed, it would force Medicare to pay for pharmacist services - just like it pays for doctors. That could unlock the full potential of expanded scope.
What’s Next?
The trend is clear: pharmacists are becoming frontline providers. By 2026, most states will allow at least some form of independent prescribing. The question isn’t if this will happen - it’s how fast and how well.
For patients, it means faster care. For pharmacists, it means using their full training. For the system, it means fewer ER visits, lower costs, and better outcomes.
If you’re on a chronic medication, live in a rural area, or have trouble seeing a doctor - ask your pharmacist what they can do for you. They might surprise you.
Can a pharmacist change my prescription without telling my doctor?
Only in specific cases. For generic substitutions, no - but they must tell you. For therapeutic interchange, they must notify your doctor in states that allow it. For prescription adaptation or collaborative practice agreements, they’re required to document the change in your health record and often send a summary to your prescriber. Independent prescribing under statewide protocols doesn’t require prior approval, but the pharmacist must still communicate the change to your primary care provider as part of standard practice.
Can I ask my pharmacist to prescribe birth control?
Yes - but only in certain states. As of 2025, California, Maryland, Oregon, Washington, New Mexico, Colorado, and Nevada allow pharmacists to prescribe birth control to adults without a doctor’s prescription. You’ll need to fill out a health questionnaire, have your blood pressure checked, and confirm you don’t have any contraindications. If you’re eligible, they can give you a 3- to 6-month supply on the spot.
Are pharmacists allowed to give me antibiotics?
In most states, no - not without a doctor’s order. But in states with statewide protocols (like New Mexico, Colorado, and California), pharmacists can prescribe antibiotics for specific conditions: urinary tract infections, strep throat, and some sinus infections - if they’ve been trained and certified to do so. They’ll test you first (like with a rapid strep test) and only treat if the diagnosis is clear. They can’t prescribe antibiotics for complex or unknown infections.
Why don’t insurance companies pay pharmacists for these services?
Because most insurance plans still classify pharmacists as dispensers, not providers. They pay for the drug - not the service. Even when a pharmacist spends 30 minutes adjusting your meds or testing for a UTI, there’s often no billing code to get paid. That’s changing slowly. The federal ECAPS Act, if passed, would create new Medicare billing codes for pharmacist services, which would pressure private insurers to follow. Until then, many of these services are offered for free or at low cost as a way to build trust and improve outcomes.
Can my pharmacist refuse to fill a prescription?
Yes - but only for very limited reasons. Pharmacists can refuse if the prescription is forged, looks like it’s being misused, or if the drug interacts dangerously with your other meds. They can’t refuse because they disagree with the doctor’s decision or because of personal beliefs - unless their state has a specific conscience clause. Even then, they must refer you to another pharmacist who will fill it. In 2025, 18 states have laws that protect patients’ access over pharmacists’ personal objections.




Allison Turner
November 27, 2025 AT 22:17This is just big pharma and chain pharmacies pushing more control so they can charge more for nothing. You think a pharmacist giving you antibiotics is saving you time? Nah. They’re just cutting the doctor out so they can upsell you on supplements and cough syrup. I’ve seen it. They’ll hand you a script for azithromycin then hand you a $40 bottle of ‘immune booster’ with 500mg of vitamin C. Same store. Same person. Same scam.
Edward Batchelder
November 29, 2025 AT 00:25As someone who’s lived in rural Nebraska for 40 years, I’ve seen the difference this makes. My wife had a UTI last winter-no doctor within 50 miles, clinic closed on Sunday, and she was in agony. The pharmacist ran a rapid test, called the on-call physician on his own time, got approval under our state’s protocol, and gave her the antibiotics before noon. He didn’t charge extra. He didn’t push anything. He just did his job. That’s not corporate greed-that’s public health. We need more of this, not less.
Gayle Jenkins
November 30, 2025 AT 23:24Let’s be real-pharmacists are the most underused professionals in healthcare. They have PhDs in pharmacology, they know drug interactions better than most GPs, and they’re the only ones who see your full med list every single time you walk in. Yet we treat them like glorified cashiers. If you’re still mad about pharmacists prescribing birth control or UTI meds, ask yourself: why does it take 3 weeks to see a doctor for a simple script when the person handing you the pills has 10x more training in drug safety than your primary care provider who’s rushing between 30 patients an hour? It’s not about scope. It’s about respect.
Darrel Smith
December 1, 2025 AT 12:18They’re taking over. They’re taking over everything. First, they swap your meds without asking. Then they start prescribing. Next thing you know, they’re ordering MRIs and running labs. Who’s watching them? Who’s holding them accountable? No one. The FDA doesn’t care. The AMA doesn’t care. And the government? They’re too busy handing out grants to pharmacy chains. This isn’t progress. This is a slow-motion power grab. One day, you’ll walk in for a cold, and they’ll hand you a prescription for antibiotics, a flu shot, a cholesterol test, and a $120 ‘wellness package’-all before you even sit down. And you’ll pay for it. Because they’ll bill your insurance like they’re a doctor. And you won’t even know the difference.
Iives Perl
December 2, 2025 AT 17:48They’re tracking you. Every pill you get. Every test they run. Every script they write. They’re feeding it all into a central database-owned by CVS and Walgreens. Next thing you know, your insurance rates go up because ‘you’re high risk’ for UTIs. Or your employer finds out you’re on birth control. This isn’t healthcare. It’s surveillance with a white coat. 🕵️♂️
Asha Jijen
December 4, 2025 AT 05:37USA always make everything complicated. In India, pharmacist give you medicine without doctor even if you say 'my head hurt' and they give you paracetamol. Why you need so many rules? Just let them help people. People suffer because of paper. No paper no problem. Simple.
reshmi mahi
December 6, 2025 AT 00:51Oh wow, so now pharmacists are superheroes?? 🦸♀️ Next they’ll be doing brain surgery and teaching kids math. At least in India, we don’t pretend a guy who counts pills is a doctor. You people turn every job into a power fantasy. 😂
laura lauraa
December 7, 2025 AT 06:15It is, indeed, a profoundly troubling epistemological rupture in the medical paradigm-a reconfiguration of professional authority predicated upon commodified access rather than clinical epistemic rigor. The pharmacists, though possessing rigorous pharmacokinetic training, lack the holistic phenomenological understanding of the patient’s existential condition, which is the very foundation of therapeutic efficacy. One cannot reduce healing to a transactional algorithm of drug substitution and protocol-driven intervention. Where, then, is the soul of medicine? Where is the physician-patient covenant? It is being dissolved-bit by bit-by the algorithmic efficiency of corporate pharmacy chains. And we, the public, are complicit in our own disenfranchisement.
sharicka holloway
December 7, 2025 AT 19:39I work in a pharmacy in Ohio and I see this every day. People come in who haven’t seen a doctor in years. They’re scared. They’re broke. They’re tired. We’re not trying to replace doctors-we’re trying to keep them alive until they can get to one. I’ve given out free insulin samples, helped someone get their blood pressure meds switched to a cheaper brand, and once stayed 45 minutes after closing to explain how to use an inhaler to a grandma who didn’t speak English. We’re not the enemy. We’re the people who show up.
Aishwarya Sivaraj
December 9, 2025 AT 03:14in india we dont have this much rules but still people get better because pharmacist know what to give if you say fever or stomach pain they give paracetamol or ors not like here where you need 10 forms and 3 referrals just for a cough. i think america needs to simplify. pharmacist are trained and they know what to do. why make it so hard for people who need help now not in 3 weeks