What Is Polypharmacy, and Why Does It Matter for Older Adults?
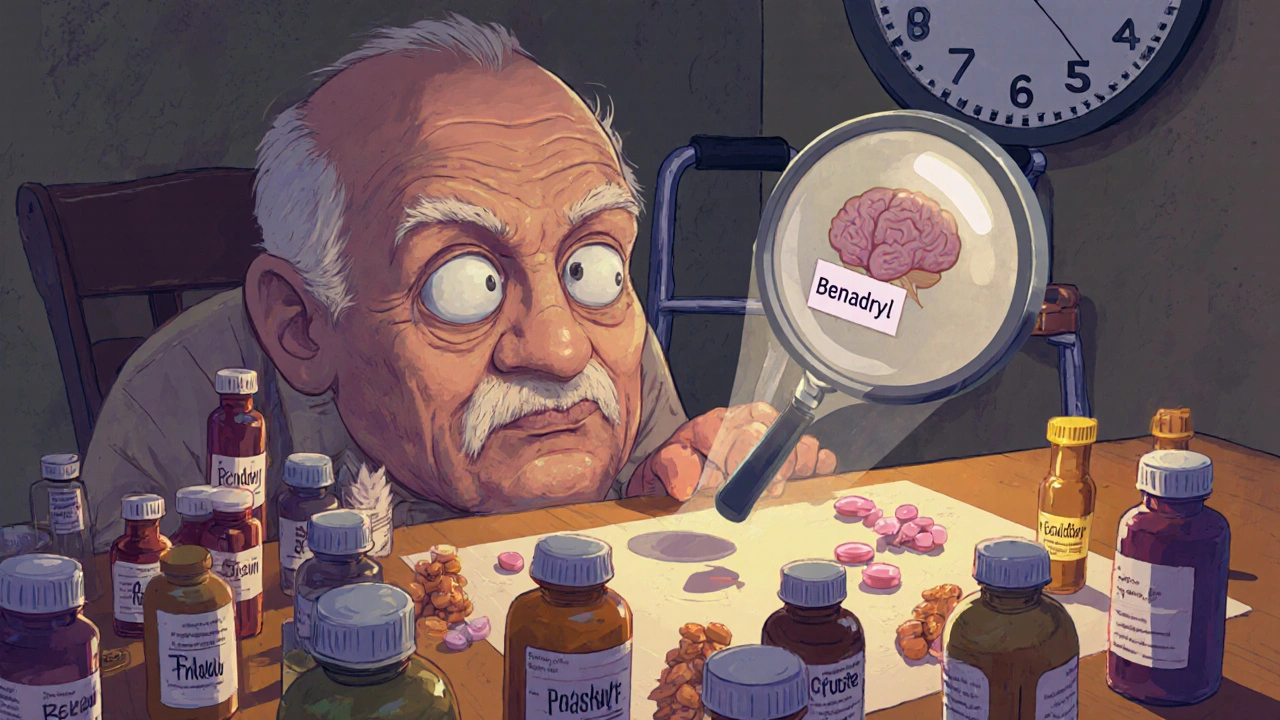
When someone takes five or more medications at the same time, that’s called polypharmacy. It’s not rare - it’s common. In New Zealand, Australia, and the U.S., nearly 4 in 10 adults over 65 are on five or more prescriptions. For those in nursing homes, the number jumps to 80%. Many of these meds are necessary - for diabetes, high blood pressure, arthritis, or heart disease. But when you stack them up, the risks start adding up faster than the benefits.
Older bodies don’t process drugs the same way they did at 30. Kidneys slow down. Liver function declines. The brain becomes more sensitive to certain chemicals. That means even a normal dose can become too strong. And when you’re taking five, seven, or ten pills a day, the chance of one drug messing with another skyrockets. By the time someone is on seven medications, it’s almost certain there’s at least one dangerous interaction hiding in the mix.
How Many Medications Are Too Many?
The number five is the usual cutoff for polypharmacy, but it’s not magic. Some people need six meds and stay healthy. Others crash on just three. What matters isn’t the count - it’s the reason. A person with heart failure, COPD, and atrial fibrillation might need five meds to survive. But if three of them are for side effects caused by another drug? That’s a prescribing cascade - and it’s dangerous.
Take painkillers. NSAIDs like ibuprofen are among the most prescribed drugs in older adults. But they raise blood pressure, hurt kidneys, and increase bleeding risk - especially when mixed with blood thinners like warfarin or aspirin. So a doctor prescribes a stomach pill to protect against ulcers. Then that stomach pill causes confusion or dizziness, so another drug is added for that. And so on. Each new med tries to fix a problem created by the last one.
Studies show that people on 10 or more drugs - called hyper-polypharmacy - are nearly twice as likely to end up in the hospital. Falls, confusion, kidney failure, internal bleeding - these aren’t just side effects. They’re often direct results of the medication pileup.
What Happens When Drugs Fight Each Other?
Drug interactions aren’t always obvious. Some are deadly. Others are silent, slowly stealing energy, memory, or balance without anyone noticing until it’s too late.
- Anticholinergics - used for overactive bladder, allergies, or sleep - block a brain chemical called acetylcholine. In older adults, this can cause memory fog, constipation, dry mouth, and even delirium. Common ones include diphenhydramine (Benadryl), oxybutynin, and some tricyclic antidepressants.
- Benzodiazepines like lorazepam or diazepam are often prescribed for anxiety or insomnia. But they increase fall risk by 40% in seniors. Combine them with opioids or sleep aids, and the risk of breathing problems spikes.
- NSAIDs + blood thinners = higher chance of stomach bleeding. Even low-dose aspirin becomes risky when paired with ibuprofen or naproxen.
- Statins + grapefruit juice - yes, even a single glass can cause muscle damage that leads to kidney failure.
And don’t forget supplements. Turmeric, ginkgo, garlic pills - they’re not harmless. Many interact with blood thinners, blood pressure meds, or diabetes drugs. A 78-year-old woman in Auckland was hospitalized after taking fish oil and warfarin together. Her INR shot up to 9.5. Normal is 2-3. She almost bled out.

Deprescribing: Stopping Meds Can Save Lives
Deprescribing isn’t about cutting pills randomly. It’s a careful, step-by-step process of reviewing every medication to ask: Is this still helping? Or is it hurting more than helping?
Think of it like cleaning out a closet. You keep the things you use. You toss the expired, the unused, the duplicates. Medications are the same. A statin might’ve been needed after a heart attack five years ago. But if the person’s now 85, has no symptoms, and takes 11 other drugs - is it still doing more good than harm?
Guidelines like the Beers Criteria and STOPP/START help doctors spot risky drugs. Beers lists medications that should usually be avoided in seniors - like long-acting benzodiazepines or certain antipsychotics used for dementia. STOPP/START goes further: it tells you what’s missing, too. Maybe someone needs a vitamin D pill but is on five unnecessary ones.
Real-world results? In one study, when pharmacists led deprescribing in nursing homes, falls dropped by 22%. Emergency visits fell. People felt more alert. Some even started walking again.
Why Is Deprescribing So Hard?
If it works, why isn’t everyone doing it?
Doctors are stretched thin. A 15-minute appointment doesn’t leave room to review 12 medications. Many haven’t been trained in deprescribing. They’re taught to add - not remove.
Patients are scared. “My doctor gave me this for my sleep - if I stop, I’ll never sleep again.” Or, “I’ve been taking this for 15 years. It must be doing something.” Many don’t know they can ask to taper off. Some think stopping meds means their condition is getting worse.
Specialists don’t talk to each other. A cardiologist prescribes a beta-blocker. A neurologist adds an anticonvulsant for nerve pain. A GP sees 14 pills on the list and doesn’t know which one to cut. No one owns the whole picture.
And then there’s the system. Doctors get paid for prescribing, not for reviewing. Pharmacies don’t flag interactions unless they’re obvious. Insurance doesn’t cover time spent talking about stopping meds.

What Can You Do - As a Patient or Caregiver?
You don’t need to wait for the system to change. Here’s how to take control:
- Make a complete list. Write down every pill, patch, cream, vitamin, and herbal supplement. Include doses and why you take them. Don’t leave out the over-the-counter stuff - antacids, sleep aids, painkillers.
- Bring it to your next appointment. Ask: “Which of these are still necessary? Are any of these causing side effects I didn’t realize?”
- Ask about deprescribing. Say: “I’m worried about taking so many meds. Can we review them together?”
- Start slow. Never stop a med cold turkey. Tapering takes time. A benzodiazepine might need weeks to reduce safely.
- Track changes. Write down how you feel before and after a med is stopped. Better sleep? Less dizziness? More energy? That’s data your doctor needs.
One man in Wellington, 82, was on 11 medications. He was dizzy, confused, and falling. His GP and pharmacist reviewed everything. They stopped three: a sleeping pill, a stomach acid reducer, and an old antidepressant. Within three weeks, his balance improved. His memory cleared. He stopped using his walker.
What’s Next? The Future of Medication Safety
Technology is starting to help. Some clinics now use AI tools that scan a patient’s full medication list and flag high-risk combinations. Pharmacists are stepping into care teams - not just filling scripts, but leading medication reviews.
Changes in payment models could help too. If doctors are paid for keeping patients healthy - not just for writing prescriptions - they’ll have more reason to cut the clutter.
But the real change starts with you. Older adults aren’t passive recipients of meds. They’re partners in their care. Asking questions, bringing lists, saying “I’m not sure I need this” - those actions save lives.
When to Call for Help
If you or someone you care for is on five or more medications and has experienced:
- Falls or balance problems
- Memory lapses or confusion
- Unexplained fatigue or weakness
- Stomach pain, bleeding, or dark stools
- Increased anxiety or depression after starting a new drug
- it’s time to schedule a medication review. Talk to your GP, pharmacist, or a geriatric specialist. Don’t wait for a crisis. Prevention is the best medicine.





Robert Bashaw
November 30, 2025 AT 11:02Jennifer Wang
December 2, 2025 AT 02:09Monica Lindsey
December 3, 2025 AT 14:54Tina Dinh
December 4, 2025 AT 17:29Steven Howell
December 6, 2025 AT 16:49Peter Axelberg
December 8, 2025 AT 07:10stephen idiado
December 8, 2025 AT 15:26Bernie Terrien
December 10, 2025 AT 12:59Subhash Singh
December 10, 2025 AT 20:41Geoff Heredia
December 12, 2025 AT 01:06Mary Kate Powers
December 13, 2025 AT 05:49Sara Shumaker
December 14, 2025 AT 02:29Brandy Johnson
December 16, 2025 AT 00:44jamie sigler
December 17, 2025 AT 06:02