When a medication changes the way your heart beats - not in a good way - it can be life-threatening. One of the most dangerous but often overlooked side effects is QT prolongation. It doesn’t cause symptoms on its own. You won’t feel dizzy or chest pain from it directly. But it’s the silent trigger behind a deadly heart rhythm called torsades de pointes, which can lead to sudden cardiac arrest. And it’s not rare. More than 200 medications - from antibiotics to antidepressants - are known to cause it.
What Exactly Is QT Prolongation?
The QT interval on an ECG measures how long it takes your heart’s lower chambers (ventricles) to recharge after each beat. This electrical reset is critical. If it takes too long - if the QT interval stretches beyond normal - your heart becomes electrically unstable. That’s QT prolongation. When the corrected QT interval (QTc) hits 500 milliseconds or more, or jumps more than 60 ms from your baseline, the risk of torsades de pointes spikes dramatically. Women are far more likely to be affected - about 70% of documented cases occur in females, especially after childbirth.How Do Medications Cause This?
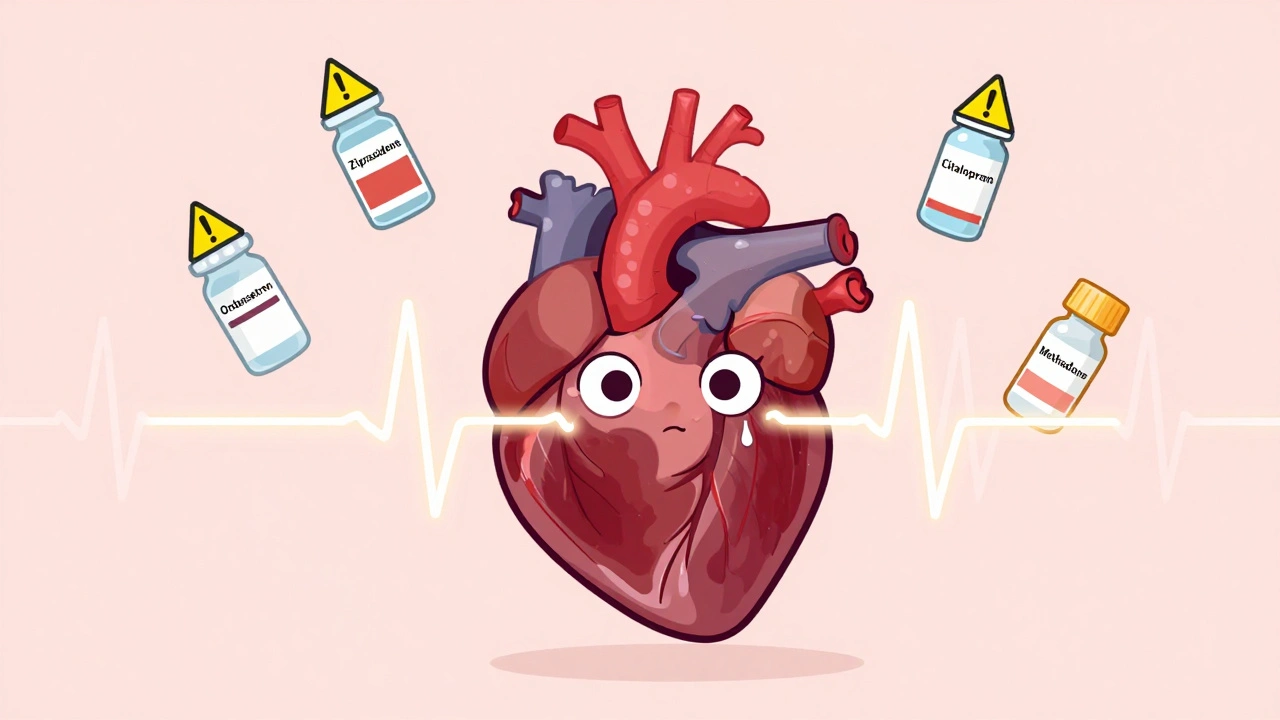
Most QT-prolonging drugs work by blocking a specific potassium channel in heart cells called hERG. This channel helps the heart reset after beating. When it’s blocked, the heart takes longer to recharge. It sounds simple, but the consequences are serious. The hERG channel is targeted by drugs that have nothing to do with heart disease. Antipsychotics like haloperidol and ziprasidone, antibiotics like clarithromycin and erythromycin, and even anti-nausea meds like ondansetron can all do it. Even common antidepressants like citalopram carry warnings. In 2011, the FDA capped citalopram at 40 mg daily (20 mg for people over 60) because higher doses reliably prolonged QTc.High-Risk Medications You Need to Know
Not all QT-prolonging drugs are created equal. Some are far more dangerous than others. Here’s who’s in the danger zone:- Class Ia and III antiarrhythmics: Quinidine, procainamide, sotalol, dofetilide. These are designed to treat arrhythmias - but they can cause them. Quinidine causes torsades in up to 6% of patients. Sotalol carries a 2-5% risk.
- Antipsychotics: Haloperidol, ziprasidone, thioridazine. Ziprasidone has a black box warning for ventricular arrhythmias. Even at standard doses, it can push QTc over 500 ms in vulnerable people.
- Antibiotics: Erythromycin and clarithromycin (macrolides) are big offenders, especially when combined with other drugs that slow their metabolism. Moxifloxacin (a fluoroquinolone) is less risky but still measurable.
- Antifungals: Fluconazole, especially at doses above 400 mg/day.
- Antiemetics: Ondansetron is one of the most common drugs linked to QT prolongation in emergency rooms. A 2020 FDA review found it involved in 42% of reported torsades cases.
- Opioid replacement: Methadone. Doses over 100 mg/day significantly raise risk. Many patients on methadone maintenance have QTc over 470 ms - but with monitoring, serious events are rare.
- Oncology drugs: Vandetanib, nilotinib, and others. Nearly half of newer cancer drugs carry QT warnings.
Why Some People Are at Much Higher Risk
It’s not just the drug. It’s the person taking it. Risk multiplies when factors stack up:- Female sex: Hormonal differences make women more sensitive to hERG blockade.
- Age over 65: Slower metabolism, more medications, weaker hearts.
- Low potassium or magnesium: Electrolyte imbalances make the heart extra vulnerable.
- Heart disease: Previous heart attack, heart failure, or bradycardia.
- Genetics: About 30% of cases involve hidden mutations in hERG or related genes. You might not know you’re at risk until it’s too late.
- Drug combinations: Taking two QT-prolonging drugs together? That’s a red flag. Haloperidol + ondansetron? That combo has caused multiple near-fatal events. Even two low-risk drugs can become dangerous in tandem.
What Doctors Should Do - And Often Don’t
The European Society of Cardiology and the American Heart Association both say: Check an ECG before starting high-risk drugs. And recheck within 3-7 days after starting or increasing the dose. But in practice, many don’t. A 2022 survey of 327 hospital pharmacists found 63% struggled to identify safe combinations. Why? Because the rules are messy. There’s no single app or checklist that tells you if your patient’s mix of meds is safe.Real Cases: When Things Go Wrong
One case from a Reddit thread in 2022 tells the story: A 65-year-old woman with stomach flu got ondansetron and azithromycin. Her QTc jumped from 440 ms to 530 ms in 24 hours. She developed torsades. She survived - barely. Her doctors didn’t check her ECG. Neither drug alone was a huge risk. Together? Deadly. Another case from 2021 showed the opposite: 87 patients on methadone for opioid addiction had their QTc monitored quarterly. None had torsades, even though 23% had QTc over 470 ms. The difference? Monitoring. Dose control. Awareness.
What’s Changing in Drug Safety
The old way of testing drugs for QT risk - just measuring QTc in healthy volunteers - is outdated. Since 2013, the FDA, EMA, and Japan’s PMDA have been using the CiPA initiative. This new approach tests drugs on multiple ion channels and uses computer models to predict arrhythmia risk. It’s more accurate. And it’s causing more drugs to fail in development. Between 2016 and 2022, 22 drugs were scrapped because of proarrhythmia risk. Each failure cost over $2.6 billion. By January 2025, all new drug applications must include CiPA data. That means fewer dangerous drugs will hit the market. But what’s already out there? That’s the problem.What You Can Do
If you’re taking any of these meds:- Ask your doctor: “Could this drug affect my heart’s electrical system?”
- Ask if you need a baseline ECG - especially if you’re over 65, female, or on multiple meds.
- Don’t take over-the-counter meds or supplements without checking. Some herbal products (like licorice root) can lower potassium and raise risk.
- If you’re on methadone, citalopram, or an antipsychotic, get your QTc checked at least once a year - or more if your dose changes.
- Know your electrolytes. Low potassium? Low magnesium? Fix those before starting a new drug.
QT prolongation isn’t something you can ignore. It’s not a rare side effect. It’s a predictable, preventable danger. The tools to stop it exist - ECGs, risk checklists, drug interaction databases like CredibleMeds.org. But they only work if you use them.
Resources You Can Use
- CredibleMeds.org: Updated quarterly. Lists every drug with known, possible, or conditional QT risk. Free for patients and clinicians. - FDA Drug Safety Communications: Search for “QT prolongation” to find latest warnings. - ECG interpretation tools: Hospitals are starting to use AI that analyzes ECGs for subtle signs of risk beyond just QTc - accuracy is now over 89%.Medication safety isn’t about avoiding drugs. It’s about using them wisely. A drug that saves your life shouldn’t end it - and with the right checks, it doesn’t have to.
Can QT prolongation happen with just one medication?
Yes. While combining drugs increases risk significantly, many single medications - like sotalol, ziprasidone, or high-dose citalopram - can cause QT prolongation on their own. The risk is higher with certain patient factors, but even healthy individuals can be affected.
Is QT prolongation always dangerous?
Not always. A slight prolongation (e.g., QTc 450-499 ms) without other risk factors rarely leads to torsades. But when QTc exceeds 500 ms, or increases by more than 60 ms from baseline, the risk jumps 3 to 5 times. That’s when action is needed.
Why are women more at risk for drug-induced torsades?
Women naturally have longer QT intervals than men, even at rest. Hormonal fluctuations - especially lower estrogen levels - make the hERG channel more sensitive to blockade. Postpartum women are particularly vulnerable due to electrolyte shifts and hormonal changes.
Can I check my QT interval at home?
No. While some smartwatches claim to detect arrhythmias, they cannot accurately measure QT interval. QT prolongation requires a 12-lead ECG interpreted by a trained professional. Home devices may miss it entirely or give false reassurance.
What should I do if I’m prescribed a QT-prolonging drug?
Ask your doctor: 1) Is this drug necessary? 2) Do I need a baseline ECG? 3) Will I need a follow-up ECG? 4) Are there safer alternatives? Don’t assume it’s safe just because it’s commonly prescribed. Your health is worth the questions.
Are there any new drugs being developed that avoid QT risk?
Yes. Thanks to the CiPA initiative, newer drugs are being screened for multi-channel effects, not just QT prolongation. Some newer antipsychotics and antibiotics are designed to avoid hERG blockade entirely. But most drugs on the market today were approved before these standards existed.
How often should I get an ECG if I’m on a high-risk medication?
Guidelines recommend a baseline ECG before starting, then a repeat within 3-7 days after initiation or any dose increase. For chronic use - like methadone or antipsychotics - an annual ECG is advised, especially if you’re over 65 or have other risk factors.




Conor Forde
December 2, 2025 AT 17:29So let me get this straight - we’re giving people drugs that can literally turn their hearts into ticking time bombs… and the only ‘safety check’ is a 30-second ECG that no one remembers to order? I’ve seen my GP prescribe azithromycin for a cold like it’s Advil. Meanwhile, my grandma’s on methadone, citalopram, and a ‘natural’ magnesium supplement that’s actually licorice root - and nobody blinked. This isn’t medicine. It’s Russian roulette with a stethoscope.
Louise Girvan
December 3, 2025 AT 11:29THEY KNOW. THEY’VE ALWAYS KNOWN. The FDA, Big Pharma, the AMA - they’ve been burying this for decades. Why? Because if patients knew how many common meds could kill them silently, they’d stop taking them. And then? The profits vanish. That’s why they push ‘monitoring’ - not prevention. They want you to die slowly so they can bill you for the ambulance, the ICU, the defibrillator… and then the funeral.
patrick sui
December 3, 2025 AT 16:07Interesting breakdown - the hERG channel blockade is definitely the core mechanism, but I’d argue the bigger issue is polypharmacy in aging populations. With 7+ meds on board, even low-risk agents (like ondansetron at 4mg) can push QTc over 500ms when combined with a CYP3A4 inhibitor like clarithromycin. The real gap? No standardized risk algorithm in EHRs. We’re still using paper checklists from 2008. CiPA is promising, but it’s not helping the 80M people already on these meds.
Declan O Reilly
December 4, 2025 AT 05:07It’s wild to think we’ve built entire industries around diagnosing cancer, diabetes, Alzheimer’s - but when it comes to the heart’s electrical rhythm? We treat it like a background noise. We measure cholesterol like it’s the end-all, but ignore the actual spark that keeps the engine running. QT prolongation isn’t a side effect - it’s a systemic failure of how we think about drugs. We treat them like pills, not electrical disruptors. Maybe we need a new word for it. Not ‘side effect.’ Not ‘risk.’ Call it ‘electrical sabotage.’
soorya Raju
December 4, 2025 AT 20:59They’re hiding the truth - the hERG channel isn’t just blocked by drugs… it’s targeted by the same corporations that own the ECG machines and the labs that ‘interpret’ them. You think they want you to catch it early? Nah. They want you to crash, then bill your insurance for the 3-day ICU stay. And don’t even get me started on how the FDA approves drugs based on ‘statistical significance’ while ignoring real-world death clusters. This is engineered negligence.
Dennis Jesuyon Balogun
December 5, 2025 AT 18:44Let me be blunt - this isn’t just about drugs. It’s about who gets care. A wealthy woman in Boston gets a baseline ECG before her antipsychotic. A single mom in Lagos gets a generic antibiotic because it’s cheap. The system doesn’t fail - it was built to fail for people like her. We need global QT-risk registries, not just FDA warnings. And we need to stop pretending that ‘monitoring’ is enough when 90% of the world has zero access to ECGs. This is a human rights issue wrapped in a pharmacology paper.
Sean McCarthy
December 7, 2025 AT 13:53Wrong. Most QT prolongation cases are preventable. The data shows 80% of torsades occur in patients with 2+ risk factors: female, >65, low K+, on 2+ QT drugs. If you’re a healthy 30-year-old male on a single low-risk med? Risk is negligible. Stop fearmongering. The real problem is doctors who don’t assess risk properly - not the drugs themselves.
Eric Vlach
December 9, 2025 AT 08:23My uncle took methadone for 12 years. QTc was always 460. No issues. He got an ECG every year. That’s it. No panic. No drama. The key is consistency. Don’t skip the checkups. Don’t mix random OTC stuff. Know your numbers. Simple. You don’t need a conspiracy. You need to show up for your own health.
Souvik Datta
December 11, 2025 AT 04:47As someone who’s worked in rural clinics across India - this is terrifyingly real. We prescribe ondansetron for vomiting, azithromycin for fever, and paracetamol for pain. No ECG. No labs. No follow-up. We don’t have the tools. But we do have the trust. So I tell patients: ‘If you feel your heart fluttering, stop everything. Walk to the hospital. Don’t wait.’ It’s not perfect. But it’s all we’ve got. We need global training, not just FDA labels.
Declan Flynn Fitness
December 12, 2025 AT 04:28Just got my annual ECG done. QTc 452. Felt good. But I’ve been on sertraline for 5 years. I asked my doc: ‘Is this safe?’ She said yes - but only after checking CredibleMeds. That’s the real win. Knowledge > fear. If you’re on meds, ask. If you’re a doc - check. We’re not helpless. We just need to stop pretending this is someone else’s problem.