You’ve had (or are about to have) cataract surgery and your surgeon mentioned fluorometholone drops. Great-now what? This guide breaks down what the drop does, when it’s chosen over stronger steroids, how to use it safely, and what to watch for so you heal well and protect your vision. I’ll keep it straight, practical, and human-exactly what I wanted when I was scheduling drop times around school pick-up for my two kids.
- TL;DR: Fluorometholone is a mild steroid eye drop used after cataract surgery to calm inflammation with a lower chance of raising eye pressure compared with stronger steroids.
- It’s often used for routine cases, for people who have had pressure spikes on steroids, or when a gentle option is enough.
- Typical dosing is 4x/day for a week, then taper over 2-4 more weeks-follow your surgeon’s exact plan.
- Watch for red flags: worsening pain, a sudden big drop in vision, pus-like discharge, halos with headache, or nausea-get urgent care.
- Many surgeons pair a steroid with an NSAID; this combo lowers swelling and cystoid macular edema risk better than steroid alone (Cochrane review, updated analyses through 2022).
What you likely want to get done after clicking this page:
- Understand what fluorometholone does-and whether it’s right for your case.
- Know exactly how to use, space, and taper your drops without messing up healing.
- Spot side effects early (especially eye pressure spikes) and know when to call.
- See how it compares to prednisolone, dexamethasone, and loteprednol.
- Get quick checklists, a simple routine, and answers to common post-op questions.
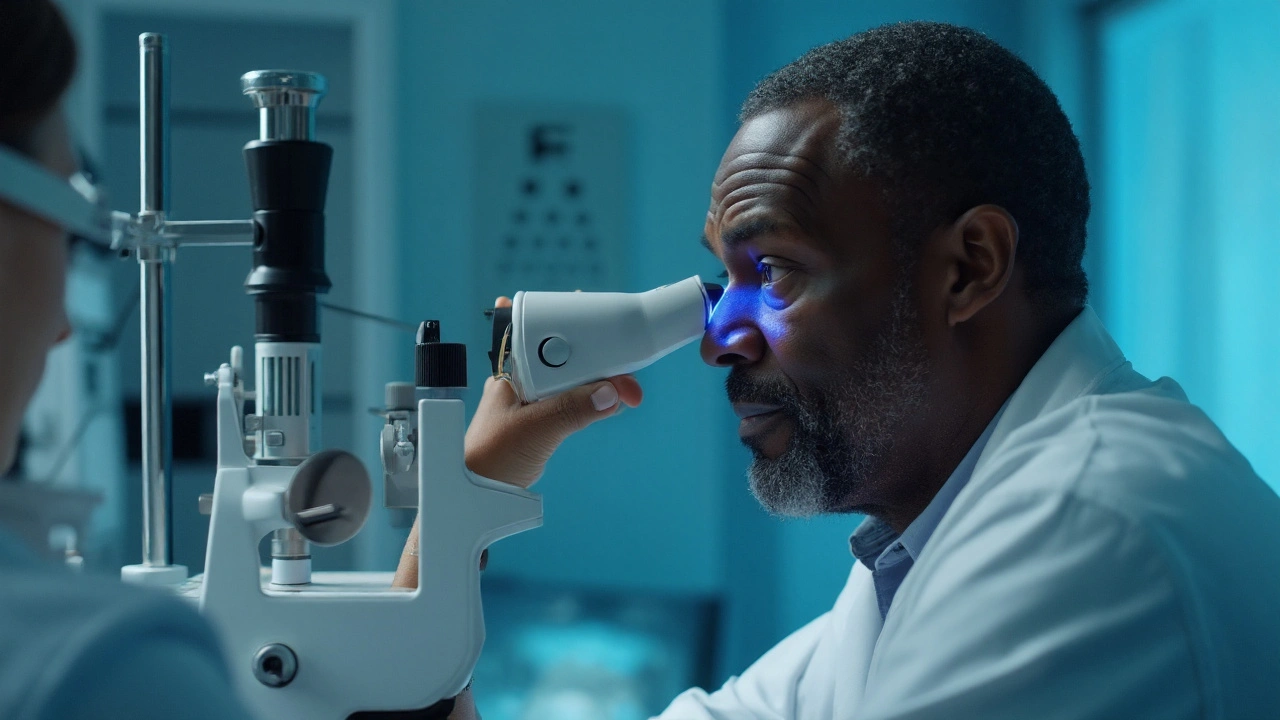
What fluorometholone does after cataract surgery (and when it’s chosen)
Fluorometholone (often labeled FML 0.1%) is a corticosteroid eye drop. After cataract surgery, your eye is inflamed from the procedure. Steroids reduce that inflammation so the cornea clears faster, vision stabilizes, and the risk of complications-like cystoid macular edema (CME)-drops.
Why this steroid, specifically? It’s a “milder” option compared with prednisolone acetate 1% or dexamethasone 0.1%. In plain terms: it calms inflammation but is less likely to raise intraocular pressure (IOP), which matters if you have glaucoma, ocular hypertension, thin corneas, or you’ve had steroid pressure spikes in the past. There are two common versions: fluorometholone 0.1% and fluorometholone acetate 0.1% (a bit stronger). Your surgeon may pick one based on how your eye looks right after surgery.
When is fluorometholone a good fit?
- Routine, uncomplicated cataract surgery with mild-to-moderate post-op inflammation.
- History of steroid response (eye pressure spike) or existing glaucoma where a gentler steroid is safer.
- Dry eye or surface irritation where you want to avoid the sting or toxicity seen with some stronger steroids.
When might a stronger steroid be chosen instead?
- Complicated surgery (e.g., longer time, iris manipulation, posterior capsule tear) or robust inflammation on day one.
- High risk for CME (e.g., diabetes, uveitis, retinal vein occlusion, epiretinal membrane) where a higher-potency steroid-or longer taper-may be better.
How good is the evidence? The American Academy of Ophthalmology (AAO) Preferred Practice Pattern for cataract surgery (2021-2023 updates) supports topical steroids post-op to control inflammation and pain. A Cochrane review (2017 with later meta-analyses through 2022) found that adding an NSAID to a steroid reduces the risk of CME compared with steroid alone. On pressure side effects, decades of data (from Armaly and Becker onward, backed by modern studies) show that potent topical steroids can raise IOP in a notable minority; fluorometholone has a lower average risk than prednisolone or dexamethasone, but not zero.
Big picture on risk: clinically significant CME after modern cataract surgery is roughly 1-2%, while OCT-detected swelling (often transient) can be higher. Post-op endophthalmitis is rare (about 0.03-0.2%), but any sudden pain and vision drop deserve urgent care. Steroid drops don’t cause infection, but they can mask it-so timing and monitoring matter.
| Drop | Relative potency | IOP rise likelihood | Typical dosing (start) | Common use after cataract | Notes |
|---|---|---|---|---|---|
| Fluorometholone 0.1% | Mild | Lower | QID then taper | Routine cases; steroid responders | Gentler on IOP; may need longer if inflammation is robust |
| Fluorometholone acetate 0.1% (e.g., Flarex) | Mild-moderate | Lower-moderate | QID then taper | Mild-moderate inflammation | More surface-friendly for some; still watch pressure |
| Prednisolone acetate 1% | High | Moderate-higher | QID-8x/day then taper | Most common for standard or higher inflammation | Gold standard potency; higher IOP risk in responders |
| Dexamethasone 0.1% | High | Higher | QID-6x/day then taper | Strong anti-inflammatory effect | More likely to raise IOP; often used in combo products |
| Loteprednol 0.5% | Moderate | Lower | QID then taper | Alternative for steroid responders | “Soft” steroid similar goal as FML; availability varies |
Availability, brands, and funding can differ by country. In New Zealand, formulations and subsidies change-ask your pharmacist what’s stocked and whether a preservative-free option is available if you’re sensitive to benzalkonium chloride (BAK).
How to use it right: dosing, tapering, combos, and safety checks
Good use beats good intentions. Here’s a simple, safe routine that fits real life.
- Wash and dry your hands.
- Shake the bottle well (suspensions need a good shake-think 10-20 seconds).
- Tilt your head back, look up, pull down the lower lid, and place one drop in the pocket. Don’t touch your eye with the tip.
- Close your eye and press gently at the inner corner (near your nose) for 60 seconds. This reduces drainage into your nose and lowers side effects.
- If you use more than one drop, wait 5 minutes between drops. If you use other drops (like an NSAID or antibiotic), wait 5 minutes between different bottles so each can work.
Typical starting schedule your surgeon might use:
- Week 1: 1 drop 4x/day (morning, lunch, late afternoon, bedtime).
- Week 2: 3x/day.
- Week 3: 2x/day.
- Week 4: 1x/day, then stop-unless told to continue.
Variations you might see:
- If inflammation is mild: a 2-3 week taper.
- If you’re high risk for swelling (diabetes, retinal disease): longer taper or a stronger steroid at first, then switch to fluorometholone.
- If you had a pressure spike on day 7: earlier switch from prednisolone to fluorometholone, plus pressure-lowering drops if needed.
Combining with other drops:
- Antibiotic: usually for the first week (or per your surgeon). Keep 5 minutes between bottles.
- NSAID (e.g., nepafenac, ketorolac, bromfenac): often used for 3-4 weeks. Evidence suggests steroid + NSAID reduces CME risk better than steroid alone; this matters if you’re diabetic or had complicated surgery.
- Glaucoma drops: keep using them unless told otherwise. Space 5 minutes from the steroid.
Missed a dose? Take it when you remember unless it’s almost time for the next dose. Don’t double up. Steroids are about steady control, not catch-up.
Don’t stop early, even if you feel great. Stopping a steroid without a taper can let inflammation rebound. Always follow the plan you were given-if you need to change it, call the clinic.
Safety checks and red flags:
- Eye pressure: steroid-induced pressure rise usually shows up between 2-6 weeks. If you’re a “steroid responder,” you know the drill-be sure you have a pressure check scheduled.
- Call urgently for: severe or worsening pain, sudden big drop in vision, light sensitivity with headache/halos, nausea/vomiting, copious discharge, or a curtain over part of your vision.
- Common annoyances: mild stinging, temporary blur after a drop, slight aftertaste. If you get significant burning, ask about a preservative-free option or a different steroid.
Practical tips to make it easy:
- Pair drop times with habits: breakfast, lunch, school pick-up, bedtime. I set phone alarms when I’m juggling the kids and dinner.
- Store at room temp away from heat. Don’t freeze.
- No contact lenses until your surgeon clears you.
- Use artificial tears (preservative-free if frequent) 10 minutes apart from your medicated drops if you’re dry or gritty.
- If you’re traveling, pack a backup bottle and a printed schedule. Airport security allows medically needed liquids-keep them in your carry-on.
Who needs extra caution?
- Glaucoma or ocular hypertension: prefer milder steroids (like fluorometholone or loteprednol), tighter pressure monitoring, and a shorter taper if possible.
- Diabetes: higher CME risk; your surgeon may combine steroid + NSAID and extend the plan.
- Herpetic eye disease history: steroids can wake herpes simplex keratitis-tell your surgeon; you may be given antiviral cover.
- Known steroid responders: expect earlier switch to milder steroid and closer checks.
Evidence and guidance notes:
- AAO Cataract in the Adult Eye Preferred Practice Pattern (latest updates through 2023): supports steroid use post-op, tailored to inflammation level and risk profile.
- Cochrane Review on NSAIDs after cataract surgery (2017; with later meta-analyses to 2022): NSAID + steroid reduces CME vs steroid alone.
- Medsafe and international safety communications: topical steroids can raise IOP; risk is dose, duration, and drug dependent.

Quick tools: checklists, scenarios, mini‑FAQ, and troubleshooting
Fast checklists you can use today.
Pre-op questions to ask (or confirm on day one):
- Which steroid am I using (exact name and %), and for how many weeks?
- What’s my taper schedule, and what might make us adjust it?
- Am I also on an NSAID? For how long?
- When is my first pressure check after surgery?
- If I notice pain or vision drop after hours, which urgent pathway do I use?
Post-op daily routine (simple version):
- Morning: antibiotic, wait 5 minutes, steroid, wait 5 minutes, NSAID.
- Midday: steroid.
- Late afternoon: steroid.
- Bedtime: steroid (+ antibiotic if still in week 1).
Symptom triage:
- Mild ache, light redness, and blur that improves day by day: usually normal-stick to the plan.
- New halos with headache, nausea, or vomiting: possible pressure spike-call urgently.
- Worsening pain, pus-like discharge, or sudden vision drop: treat as urgent until proven otherwise.
- Persistent blur past 3-4 weeks or new central blur: ask about macular swelling (OCT can check).
Scenarios and what to do:
- You’re a known steroid responder: ask if starting directly with fluorometholone (or loteprednol) is better for you, and schedule an early IOP check (often day 7-10).
- Diabetic with retinal disease: you may need the combo (steroid + NSAID) longer. Clarify exact duration.
- Significant corneal swelling on day one: don’t panic-often settles in days. Your surgeon might keep a stronger steroid a bit longer before switching to fluorometholone.
- Preservative sensitivity: ask for preservative-free steroid options or dosing strategies that reduce BAK exposure.
Mini‑FAQ
- Is fluorometholone strong enough on its own? For many routine cases, yes. If inflammation runs high, your surgeon may start stronger then step down to fluorometholone.
- How long will I use it? Commonly 3-4 weeks with a taper. Some need shorter; some (especially higher risk eyes) need longer.
- Does fluorometholone raise eye pressure? It can, but on average less than prednisolone or dexamethasone. About 5% of people are high steroid responders; glaucoma patients are more likely to spike. That’s why pressure checks matter.
- Can I drive while using it? If your vision meets legal standards and you feel safe, yes. Early on, glare and blur can be bothersome-only drive when you’re confident.
- Can I use it with my glaucoma drops? Yes-space them 5 minutes apart. Tell your surgeon all the drops you’re on.
- Will it cause cataracts? Long-term steroids can cause cataracts in natural lenses, but the operated eye has an artificial lens, so that specific risk isn’t a concern for that eye.
- What if I feel fine-can I stop early? Don’t. Steroids need a taper to prevent rebound. Check with your surgeon first.
- What if I forget the bottle at work? Missing a dose or two rarely ruins outcomes. Resume as soon as you can and keep to the schedule.
Troubleshooting by persona
- Routine, low-risk patient: fluorometholone QID tapering over 3-4 weeks; pair with NSAID if recommended; one pressure check in the first few weeks.
- Steroid responder/glaucoma: start with fluorometholone (or loteprednol), shortest effective taper, early IOP check, and have a plan if pressure rises (e.g., add timolol per clinician).
- Diabetic or macular risk: don’t skip the NSAID; expect a longer course; book a macular OCT if vision lags or distortion appears.
- Surface-sensitive/dry eye: consider preservative-free formulations and more frequent lubricants spaced 10 minutes away from medicated drops.
Cost and access tips (NZ-friendly):
- Brands and funding change-ask your pharmacist what’s currently subsidised and if a switch is reasonable for you.
- If out-of-stock, ask the clinic for an approved alternative (loteprednol or prednisolone with closer pressure checks).
Key rule of thumb: stronger inflammation needs stronger steroids or longer tapers. Higher pressure risk needs gentler steroids and more monitoring. Your exact plan should reflect both.
If you remember one thing from this page, make it this: follow the taper, show up for the pressure check, and call if pain or vision go the wrong way. That’s how you get the clear, crisp vision you signed up for.




George Ramos
September 14, 2025 AT 12:35So let me get this straight - we’re giving people steroid drops after eye surgery, and the FDA’s just shrugging? 😏 Meanwhile, Big Pharma’s laughing all the way to the bank while we’re blindfolded with a 4x/day schedule that looks like a cult ritual. Fluorometholone? More like Fluoro-MINDCONTROL. They don’t want you to know that 1 in 5 steroid responders end up with permanent IOP damage… and the ‘taper’? Just a polite way to say ‘we’ll let you go blind slowly.’ 🕵️♂️👁️🗨️
Barney Rix
September 16, 2025 AT 08:26While the post provides a clinically structured overview of fluorometholone usage, several key methodological omissions warrant attention. The comparative efficacy data presented lacks standardized units for intraocular pressure (IOP) elevation, and the Cochrane meta-analysis referenced is not explicitly cited with DOI or versioning. Furthermore, the absence of confidence intervals for the 1–2% CME incidence rate undermines statistical rigor. A proper risk-benefit analysis would require stratification by baseline IOP, corneal thickness, and prior steroid exposure - none of which are addressed. In sum, while pragmatically useful, this guide lacks the granularity expected in peer-reviewed clinical guidance.
juliephone bee
September 17, 2025 AT 19:21hi i just had cataract surgery last week and im using fluorometholone… i think i might be one of those people who gets pressure spikes? my eye feels kinda weird after the 3rd drop of the day. i dont wanna be annoying but… is it normal to feel like your eyeball is a balloon? also i forgot to press the corner of my eye once… did i mess up? 🥲
Ellen Richards
September 19, 2025 AT 11:11OMG I’m so glad I found this!! 🥹 I’ve been using this stuff since my surgery and honestly? I felt like such a failure when I forgot a dose because I was chasing my toddler around the house. But now I know I’m not alone!! And I just bought the preservative-free version because my eyes were burning so bad I cried in the shower 😭 (not even joking). Also, I’m totally doing the NSAID combo now - if you’re not doing it, you’re basically leaving your vision on ‘low quality’ mode. 💅👁️✨
Renee Zalusky
September 21, 2025 AT 00:11Wow. This is… surprisingly poetic for a medical guide. The way you framed it - like a quiet conversation over coffee after a long day - made me feel less like a patient and more like a person. I’m a diabetic with a history of macular edema, and I’ve been terrified of steroids since my last surgery. But reading this, I actually feel… hopeful. Not because it’s sugar-coated, but because it’s honest. And I’m going to print this out and tape it to my bathroom mirror. Thank you. 🌿
Scott Mcdonald
September 21, 2025 AT 17:41Hey! I just had my surgery last Tuesday and I’m on fluorometholone too! You said to use it 4x a day - but what if I’m at work and can’t drop it at lunch? Can I just do it when I get home? Also, my dog licked my bottle once… is it ruined? Should I panic? 😅
Victoria Bronfman
September 22, 2025 AT 02:02YAS QUEEN 🌟 I’m so here for this! Fluorometholone? More like FABULOMETHOLONE 💅✨ I’ve been using it since my surgery and my vision is *crystal* - like, I can read the tiny print on my coffee cup again! And guess what? I’m using the preservative-free version with my fancy eye drops organizer 🥰✨ Also, I got a cute little bottle charm to match my outfit. Because why should healing be boring? 🌈👁️💖
Gregg Deboben
September 23, 2025 AT 03:18Listen up, America - this is what happens when you let foreigners write your medical guidelines. Fluorometholone? That’s a British compromise drug. Real men use prednisolone. You want your vision sharp? You don’t taper - you *dominate*. And if you’re scared of a little pressure spike, maybe you shouldn’t have had the surgery in the first place. This country used to be strong. Now we’re giving out mild steroids like lollipops. 🇺🇸👁️💥
Christopher John Schell
September 25, 2025 AT 03:09You got this! 💪 I know it feels overwhelming with all the drops and timing, but you’re doing AMAZING. Seriously - just take it one drop at a time. Set those alarms, celebrate each day you stick to the plan, and remember: your eyes are healing because YOU showed up. I’ve helped 12 people through this exact process - you’re not alone. And hey - if you miss a dose? No biggie. Just breathe, reset, and keep going. You’re not failing - you’re FIGHTING. 🙌👁️✨
Felix Alarcón
September 26, 2025 AT 18:13Hi there - i’m from mexico but live in texas now, and i just want to say thank you for writing this in a way that actually feels human. in my home country, we’re often given a single bottle and told ‘use it twice a day’ with no taper, no explanation. i cried reading your line about pairing drops with school pick-up - that’s my life too. i’m diabetic and scared, but now i feel like i can talk to my doctor without shame. you made me feel seen. 🌎❤️
Lori Rivera
September 27, 2025 AT 08:32While the clinical content presented is generally accurate and well-structured, the tone of the post - while intended to be accessible - occasionally undermines its own authority through colloquialisms such as 'Great-now what?' and 'I’ll keep it straight, practical, and human.' In formal clinical communication, particularly in ophthalmology, precision and neutrality remain paramount. The inclusion of personal anecdotes, while relatable, may inadvertently reduce perceived objectivity among peer clinicians or regulatory reviewers. A more balanced approach would retain clarity without sacrificing professional register.
Leif Totusek
September 28, 2025 AT 17:11Fluorometholone’s relative potency is well-documented in the literature, but the assumption that a milder steroid is inherently safer for all patients is not universally valid. In patients with subclinical inflammation or delayed healing, under-treatment may prolong recovery or increase the risk of fibrosis. The tapering schedule provided is appropriate for low-risk cases, but the absence of biomarkers - such as anterior chamber cell grading or OCT-derived macular thickness - renders the protocol protocol-dependent rather than patient-dependent. Clinical judgment remains irreplaceable.